Unusual Case of Nasopharyngeal Carcinoma with Intracranial Metastasis without Direct Invasion-Juniper Publishers
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
Unusual Case of Nasopharyngeal Carcinoma with Intracranial Metastasis without Direct Invasion
Abstract
Intracranial metastasis from Nasopharyngeal Carcinoma (NPC) is an extremely rare occurrence, although direct intracranial invasion is not infrequent in patients with NPC at a locally advanced stage. Only a few patients have been reported in detail in the English literature. Here, we report a case of a man with left high parietal dural metastasis of NPC, detected 2 years after Completed Concurrent Chemoradiotherapy (CCRT).
Introduction
Nasopharyngeal Carcinoma (NPC) is a rare malignancy in Western countries but considered endemic in certain places such as southern China and Southeast Asia [1] In Malaysia, NPC is the fifth (4.9%) most common cancer among Malaysians and the third (8.1%) most common cancer among males [2]. Because of nasopharyngeal anatomical location, patients with locally advanced NPC, it is not infrequent that the primary tumor directly invades the intracranial sites such as cavernous sinus through the skull base. Distant metastases to Central Nervous System (CNS) either through hematogenous route or Cerebral Spinal Fluid (CSF) spread are rare and dural metastasis at parietal region is even extremely rarer [3]. In this article, we report a rare of an elderly man with left parietal dural metastasis from NPC.
Case Report
A 65-year-old male was diagnosed with T2N1M0-Stage II NPC (American Joint Committee on Cancer (AJCC, 7 edition)) back in 2015. A Magnetic Resonance Imaging (MRI) scan and fiber optic endoscopy revealed a small primary tumor in left lateral nasopharynx and the biopsy revealed undifferentiated carcinoma of the nasopharynx. There was no intracranial extension but presence of metastatic lymph node measuring 1.5cm in greatest dimension over right neck. Three cycles of cisplatin based combined chemotherapy regimen (cisplatin, 5-flourouracil) were given prior to radiotherapy and a complete response was obtained at both primary site and in the neck. The nasopharynx and regional lymphatics were treated to a total dose of 34 fractionwith conventional radiotherapy regimen. He subsequent received a Concurrent Chemoradiotherapy (CCRT), which was finally completed in May 2017. Patient had been on surveillance follow up with Oncology team since then.
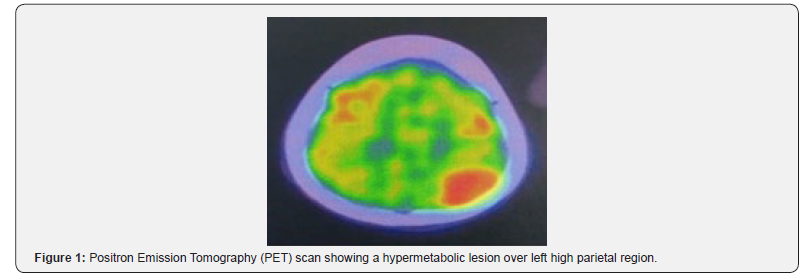
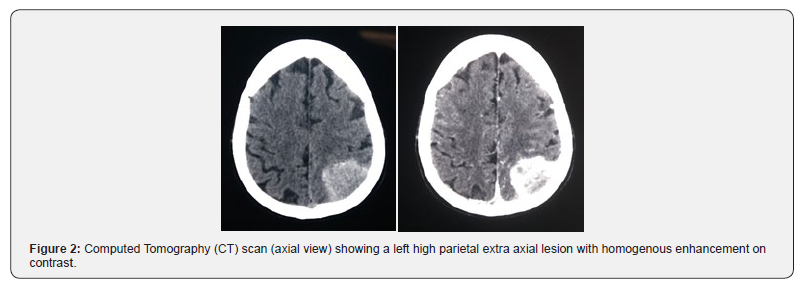
He remained well until 2 years after the conclusion of the radiotherapy, when he presented with pain over the left chest region for which a Computed Tomography (CT) Thorax was performed at a private center. On assessment, there was no neurological deficit elicited during that time. On CT imaging, there was nodular left pleural thickening with enhancement with metastasis lesions in thoracic vertebral bodies. Fluorodeoxyglucose positron emission computed tomography (FDG-PET/CT) scan was done for detailed workup, revealed pathological uptakes at the left nasopharynx, left pleural, left lung and a new hypermetabolic hyperdense mass in left higher parietal lobe, measuring 4.5 x 3.2 cm in size (Figure 1). The extra axial mass enhanced homogenously at a contrasted enhance CT with minimal edema (Figure 2). Radiologically unable to rule out possibility of a convexity meningioma arising from left parietal dura. The brain lesion was excised totally with a craniotomy and pathological examination revealed metastatic undifferentiated carcinoma (WHO Grade III).
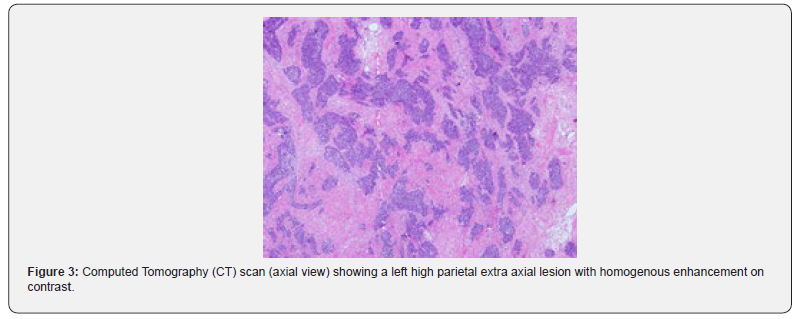
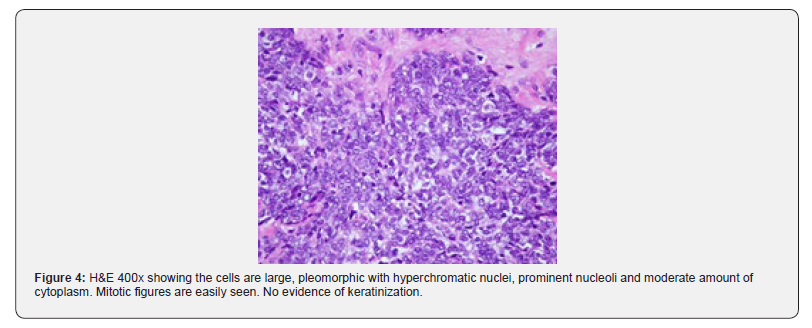
On microscopic examination, the tumor shows fragments of cellular tissue infiltrated by malignant tumor arranged in syncytial pattern of cohesive cells with indistinct cell margins. The cells were large, pleomorphic with hyperchromatic nuclei, prominent nucleoli and moderate amount of cytoplasm. There was focal necrosis, and high mitosis. Immunohistochemical study revealedthat the tumor cells showed membranous CK 5/6 (Cytokeratin 5/6) immunoreactivity (Figure 3&4). Original diagnosis of the nasopharyngeal mass made in 2015 was confirmed to be undifferentiated nasopharyngeal carcinoma, which has similar morphological characteristics as the metastatic carcinoma to the brain. Post-operative, he was right hemiplegic secondary to infarct with hemorrhagic transformation. Patient was opted for palliative care in view next line of chemotherapy is high risk for the patient with current poor performance status.
Discussion
Even though intracranial invasion by direct extension of locally advanced disease is not uncommon, metastases to the CNS, either through hematogenous route or through the Cerebrospinal Fluid (CSF), from NPC have rarely been reported. Metastatic lesions to occipital and temporal lobes have been reported in some cases but for this gentleman, metastatic lesion was located near the parietal lobe [4, 5]. There is no known lymphatic or vascular connection between the nasopharynx and parietal lobes. Ngan and colleagues, discussing the same issue for the patients who had occipital metastases, hypothesized that microenvironment in the occipital lobes might have facilitated the metastatic tumor cells to localize in that region [5]. This case has shown that the occipital lobe and temporal are not the only sites for NPC cells to metastasize, thus make this case the first to be reported of a parietal dural metastasis from NPC. The incidence of recurrence of NPC has been reported as high as 77.5% following a remission, in which 48.1% occurs after 2 years while 17.4% recurred after 7-12 months [6]. Concurrent Chemoradiotherapy (CCRT) is the most potent treatment combination for locoregional control as well as improve overall survival for the advanced disease [7]. However, the impact of CCRT upon distant control was inadequate [8]. As for this case even with a good locoregional control post CCRT, yet after 2 years patient develop new distant metastasis to lung, vertebral bodies and brain. The 5-year overall survival rate of non-metastatic locoregionally advanced NPC treated with radiotherapy is reportedly up to just 60%, while the presence of distant metastases decreases it further to be around 12-15 months at best, after chemotherapy [9].
Status of primary tumor, evidences of disseminated disease, performance status of the patient, treatment modalities already applied to the patient, histopathology of the tumor, and symptoms related to brain metastases are the factors effecting the therapeuticmanagement. Since there was locoregional recurrence and patient was hemiplegic after operation, palliative care was planned for this patient. Palliative chemotherapy was not given in view his family members refused. In conclusion, due to the rarity of dural metastasis from the NPC, a high index of suspicion should be practiced where 6 monthly or yearly radiological assessments should be performed to rule out distant metastases including a CT scan of the brain.
For more articles in Open access Journal of Head Neck & Spine Surgery | please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf

Comments
Post a Comment