Study of Laryngotracheal Stenosis and its Management in 25 Cases-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Introduction: Laryngotracheal stenosis is a
complex problem resulting most often from intubation, trauma, or
autoimmune disease. In this modern era, airway trauma has increased by
considerable number owing to increased ventilator care in many emergency
situations [1].
Anaesthetist's timely intubation saves the life of a patient but he
must also be able to foresee the chaotic life of a prolongedly intubated
patient who might develop stenosis.
Objectives of the study: Clinical study of LTS
was done to observe the various etiological causes for it and major
concentration was towards the post intubational stenosis. With
increasing ventilatory support for varied reasons in present day
intensive care setup, the incidence of stenosis following intubation has
equally increase. Management of these cases needs a great surgical
expertise, due to high failure rate as well as many complications.
T-tube stenting has shown to be relatively easier modality of surgical
treatment and it has also sub serves the purpose of regaining voice
producing ability after tracheostomy. Apart from observing other types
of treatments, T-tube stenting, its complications, their management and
results have been studied.
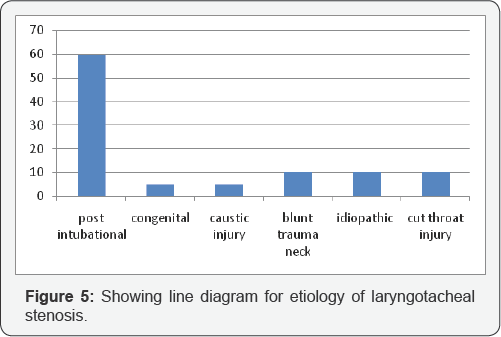
Results: Out of 25 cases that were studied
12(48%) were males and 13(52%) were females, showing no significant
sexual preponderance.Out of 25, there were 4 pediatric cases ageing
below 12 years. Speaking of aetiology, post intubational stenosis is the
cause in 64%. Reasons for intubation being diverse from blunt trauma
(8%), congenitall (4%), and caustic ingestion induced stenosis (4%),
after repair of cut throat injury (20%), idiopathic stenosis (8%).
Infectious diseases as cause in 8% and organophosphorous poisoning in
36%. Subglottis and proximal trachea were the most common sites for
stenosis, followed by distal trachea, glottis and supraglottis in the
descending order. Out of 25 cases, 2 cases were followed conservatively
without tracheostomy, 4 cases were managed conservatively with
tracheostomy, 17 cases were managed surgically definitively and death in
2 cases. Various surgical modalities used were laser excision (2
cases), T tube stenting (13 cases), Radiofrequency ablation (1 case) and
resection and reconstruction in 1 case. Out of 17 surgically managed
cases, failure was seen in 4 cases.
IntroductionPathophysiology
The recommended limits to minimize damage to the
trachea are 15-25cm H2O (10-18mmHg). Tracheal capillary pressure lies
between 20 and 30mmHg [2].
It suffers impairment at 22mmHg and total obstruction at 37mmHg. In
intubated patients Endotracheal tube cuff pressure being exerted on the
tracheal wall, becomes the main culprit in majority of the cases.
Complications of continued cuff over inflation include tracheal
stenosis, trachealmalacia, and tracheosophageal or tracheoinominate
fistula, desensitisation of the larynx and potential loss of the cough
reflex.
Poiseuille's law
a) R = resistance
c) l = length
d) r = radius
[Because of the fourth power in the denominator, resistance increases rapidly as diameter decreases] [3].
Thus, this equation proves how the tracheal lumen narrowing by stenosis affects resistance.
The process of post-intubation tracheal stenosis is
best described as the laryngotracheal bed sore. Transient irritation of
tracheal wall by the tube results in edema which heals spontaneously.
High pressure cuffs may cause ulceration of mucosa which initiates
healing process leading to tracheal stenosis which may take 3-6 weeks.
There are many factors that can lead to
laryngotracheal stenosis (LTS). Most cases of adult LTS result from
external trauma or prolonged endotracheal intubation. External trauma
causes cartilage damage and mucosal disruption with hematoma formation.
These hematomas eventually organize and result in collagen deposition
and scar tissue formation. Endotracheal intubation can cause direct
injury, and mucosal damage through pressure necrosis can result from the
pressure ofthe endotracheal tube or cuff. Mucosal ulceration also leads
to healing through collagen deposition, fibrosis, and scar tissue
formation. Lesions from endotracheal intubation are usually located in
the posterior part of the glottis, where the tube most often contacts
mucosa, or in the trachea, where the cuff or tube tip causes mucosal
damage. Low-pressure endotracheal tube cuffs have somewhat reduced the
rate of cuff-induced damage. The length of intubation, tube movement,
tube size, and gastroesophageal reflux can also contribute to the
development of LTS [4,5].
Tracheal stenosis can present very insidiously or as
a catastrophic near death episode requiring cardiopulmonary
resuscitation. Children with congenital tracheal stenosis present with
biphasic stridor, tachypnoea, retractions, nasal flaring, apnea,
cyanosis, wheezing, noisy breathing, persistant croup and pneumonia.
Dysphagia and failure to thrive may be seen occasionally [6].
Patients with acquired stenosis are diagnosed from a few days to 10 years or more following initial injury [7].
Majority are diagnosed within a year; some are misdiagnosed with asthma
and recurrent bronchitis. High index of suspicion should arise when
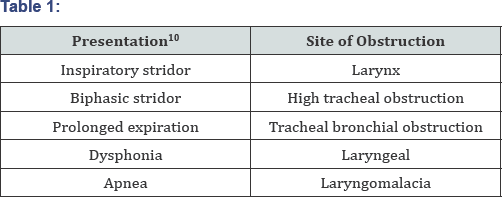
history of intubation is noted [8,9] (Table 1).
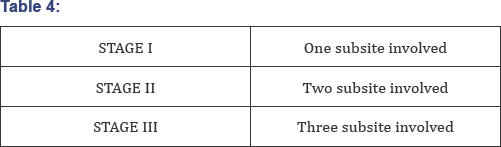
Classification
The Myer-Cotton staging system [11]
is useful for mature, firm, circumferential stenosis confined to the
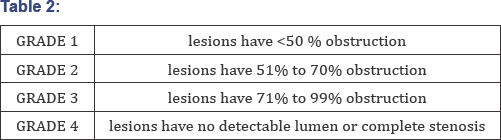
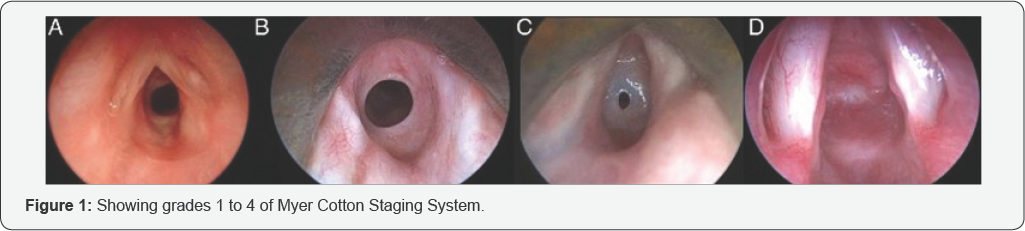
subglottis. Four grades of stenosis are described with this system: (Table 2) (Figure 1).
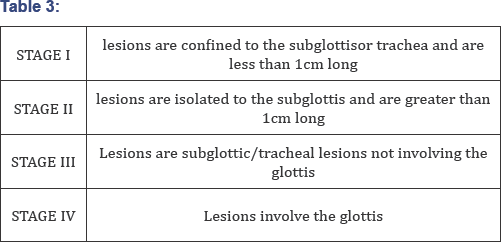
The McCaffrey system [12]
classifies laryngotracheal stenosis based on the sub sites involved and
the length of the stenosis. Four stages are described (Table 3).
The evaluation of LTS must begin with a meticulous
history and physical examination. Since most cases of LTS result from
laryngotracheal trauma or endotracheal intubation, the timing of the
predisposing incident should be recorded. The entire upper aerodigestive
tract must be carefully examined in a patient with suspected LTS [14,15].
Indirect laryngoscopy and flexible fiberoptic laryngoscopy offer
critical information regarding the supraglottic airway and mobility of
the true vocal folds [16].
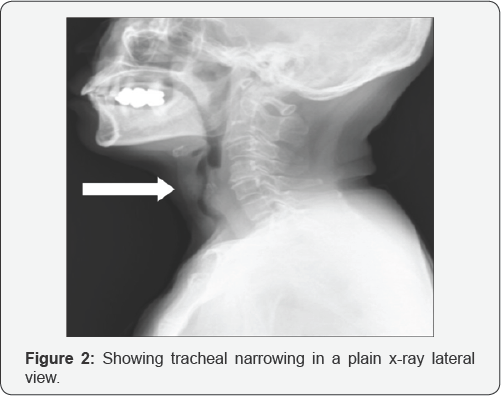
The anteroposterior airway is superb for examining
the glottic and subglottic areas. Cross-sectional imaging also
adequately shows the airway. Configuration of the airway on axial or
transverse images varies depending on the level of the image. At the
level of the epiglottis and aryepiglottic folds, the airway is elliptic.
Approaching the false cords, the airway narrows and assumes a teardrop
shape. The airway becomes elliptic at the true cords. Below the cricoid
cartilage, the airway appears circular. The posterior membrane of the
trachea may posteriorly flatten, and the normal esophagus occasionally
indents the airway silhouette [17] (Figure 2).
Although imaging studies such as airway radiographs,
computed tomography, and magnetic resonance imaging occasionally provide
useful information, the most valuable diagnostic assessment stems from
the examination of the patient with endoscopy, either flexible fibre
optic or rigid endoscopy.
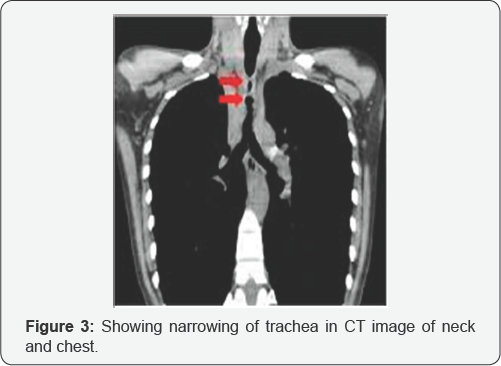
CT, MRI, VIRTUAL BRONCHOGRAM are equally useful
radiological investigation to reconstruct the images of airway in 3d
format. Technological advances in CT scanning and MRI have greatly
improved radiologist's ability to image the upper airway Spiral CT
scanning and fast MRI techniques allow the use of rapid acquisition
speeds that decrease degradation motion artifacts caused by patients
breathing and swallowing and carotid artery pulsations. Spiral CT
scanners rapidly, in less than 10 seconds, acquire the complete data set
through the larynx, limiting the time during which the patient needs to
remain motionless. Images can then be reconstructed to create
overlapping sections, and coronal, sagittal, and even 3-D images can be
generated from the same data set [18].
Helical
CT scanning with 3-D reconstruction and virtual endoscopy in neonates
and infants can prevent additional diagnostic tracheobronchoscopyin a
high percentage of such patients who have tracheobronchial lesions (Figure 3).
Medical
Prior to airway reconstruction, it is recommended that all pediatric patients be evaluated for GER with a dual 24hr pH probe [11].
In adults it is important to evaluate the patients general medical
condition prior to performing any reconstructive procedures. It is
important to consider each patient's case on an individual basis and
make the decision to proceed with surgery based on sound
judgment.Relative contraindications to LTR in adults are renal failure,
diabetes, severe coronary artery disease, severe COPD or restrictive
lung disease, obstructive sleep apnea, and systemic steroid use [19].
Patients (children and adults) with Cotton-Myer grade
I and mild grade II subglottic stenosis may sometimes be managed with
close observation (Walner and Cotton, 1999).
Surgical treatment options for subglottic stenosis:
a) Tracheostomy
b) Endoscopic
i. Dilation
ii. Endoscopic laser excision
c) Open procedure
i. E xpansion procedure27 (one-stage or with stent placement)
a. Anterior cricoid split +- cartilage graft
b. Posterior cricoid split +- cartilage graft
c. Anterior and posterior cricoid split + cartilage graft
d. Four quadrant LTR
ii. Segmental resection (cricotracheal resection - CTR)
A. Primary CTR
B. Salvage CTR
C. Extended CTR
Endoscopic treatment
Some areas of LTS are amenable to endoscopic
treatment techniques such as laser vaporization and dilation, excision
using a microtrapdoor technique, or serial dilation with radial
incisions of the stenotic segment. Intralesional corticosteroids may
also be injected under endoscopic guidance [20].
Owing to its precision (small spot size) and
availability, the carbondioxide laser, which produces light in the
mid-infrared region, remains the instrument of choice in the endoscopic
management of LTS. It can be used to coagulate vessels up to 0. 5mm in
diameter. If the stenotic area is vascular, a laser with better
hemoglobin absorption, such as the potassium titanyl phosphate/532
(KTP/532) or neodymium: yttrium-aluminum garnet (Nd:YAG), is recommended
[21].
Severe areas of LTS that do not respond to endoscopic
techniques require an open surgical procedure. Open techniques attempt
to either excise the stenotic segment and reanastomose the airway or
augment the circumference of the stenotic segment with transplanted
tissue. In the high risk patients, a tracheostomy may be the most
prudent choice of management.
Areas of cervical tracheal stenosis up to about 5cm
can generally be excised, and the proximal and distal tracheal segments
reanastomosed primarily.
Laryngeal and tracheal stents are solid or hollow
absorbable or nonabsorbable tubes of various shapes, sizes, and
materials. Stents are used as primary treatment for lumen collapse or to
stabilize a reconstructive effort of the larynx or trachea to prevent
collapse.
Types of stents [20]:
Different stents have different indications. Types include primarily
laryngeal stents, primarily tracheal stents, combination tracheal and
laryngeal stents, and stents that can be used either in the larynx or
trachea.
Laryngeal stents: If stenosis is confined to
the larynx (i.e., glottis, subglottis), stenting can be short- or
long-term. Shortterm stenting is defined as stenting for less than 6
weeks. Longterm stenting is defined as stenting for more than 6 weeks.
Use short-term stenting for stabilization of cartilage grafts following
laryngotracheal reconstruction (LTR) and/or for separation of mucosal
surfaces during healing following laryngeal trauma, repair of web
formation or atresia, or excision of a laryngeal lesion. Stents for
these indications include Aboulker stents, silicone stents, Montgomery
laryngeal stents, endotracheal tubes, and laryngeal keels (Figure 4).

Occasionally, long-term stenting is required when the
trachea above the tracheotomy tube requires stenting for either
collapse or stenosis following reconstruction. In this case, a long
stent wired to the trachea, shown in the images below, or a tracheal
tube (T-tube), such as the Montgomery T-tube, shown below, can be used.
This study is conducted at GOVT.ENT HOSPITAL, KOTI,
Hyderabad between 2012 october & 2016 January. A total number of 25
patients were studied among which 12 were males and 13 were females.
Only 4 children (below 12 years) were among the group. All the patients
presenting with strid or, difficulty to breathe (Patients with malignant
tumors of airway, Foreign bodies in air passage and paralytic
conditions of the vocal cords were excluded from the study) were
evaluated.
Among the 25 patients with airway obstruction due to
airway stenosis evaluated, majority of the patients presented with
history of intubation for various reasons highlighting the crux of
intubation hazards on airway. 5 cases presented with traumatic history
{2 blunt trauma and 3 cut throat injury}. One rare case of congenital
stenosis with aberrant subclavian artery is noted. Two cases showed
marked stenosis due to granulomatous diseases. All patients presented
with shortness of breath (progressive in some and acute onset in few
cases) necessitating the role of tracheostomy.
Bronchoscopic evaluation was the investigation of
choice and x ray neck aided further in diagnosis. Role of CT neck and
virtual bronchogram was limited and the patients included in this were
from a lower socioeconomic class who could not afford those costly
investigations. In 2 patients of lowtracheal stenosis, emergency
tracheostomy could not serve the purpose where we had to loose the
patients. Tracheostomy saves the patient's life and also relieves
him/her from the dyspnoea and stridor, but only at the cost of loss of
speech, which now becomes the major desire for the patient.
In a patient of supraglottic stenosis due to caustic
ingestion difficulty in swallowing, occasional coughing and
breathlessness on exertion were present. She was followed up by
regularly without any intervention and the patient is doing well. 2
patients of glottis stenoses (laryngeal web) were addressed by LASER
followed by keel placement for 6weeks and they are doing well. 2
patients of idiopathic stenosis on tracheostomy were managed by
steroids.
Resection and anastamosis was done in one case in the
hands of a well trained surgeon and patient is normal at follow ups.
Rest all cases owing to patient's desire of regaining voice producing
ability, surgeon's choice, patient's affordability; MONTGOMERY T-tube
stenting was done. Of which, 9 patients showed good response while 4
suffered from granulations from walls of airway Topical application of
mitomycin C after surface removal of these granulations showed good
results in these cases along with steroid nebulisations. Frequent follow
up of these stent patients was done using a 70 degree endoscope to
visualize both upper and lower ends of the tube. Cases were followed up
regularly after discharge until decanulation. T tube was maintained for
atleast an year to 18 months before decannulation.
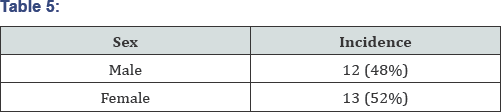
Out of 25 cases that were studied 12(48%) were males
and 13(52%) were females, showing no significant sexual preponderance.
Out of 25, there were 4 pediatric cases ageing below 12 years (Table 5).
Aetiology
There were varied causes for the development of
stenotic airway among which post intubational stenosis was predominant.
It shares 64% of the incidence. Reasons for intubation being diverse,
its role is not significant. One case of congenital origin and one case
of caustic ingestion induced stenosis was reported. 2cases each of blunt
trauma induced and idiopathic induced stenosis were noted. And 3 out of
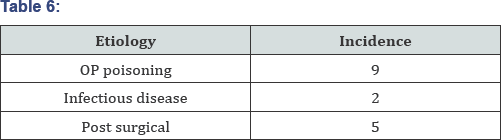
25 cases developed after repair of cut throat injury (Figure 5). When the history for intubation was taken statistics obtained are as follows... (n=16) (Table 6).
Site of lesion
Supraglottis, glottis and subglottic areas are
subsites of larynx while trachea has been classified as proximal and
distal trachea i.e with reference as 6th tracheal ring. Depending on the
nature of etiology, site of lesion varies (Figure 6).
[As most of subglottis lesions were associated with proximal tracheal
lesions, they are combined with subglottic lesions while distal lesions
are separately listed.]

Nature of lesion
Subglottis and trachea being slightly ovoid
structures stenotic segments were mostly circumferential, very few were
partial and also pinhole type of stenoses. Glottis lesions were in the
form of anterior webs. Supraglottis was distorted due to multiple
adhesions to surrounding structures.

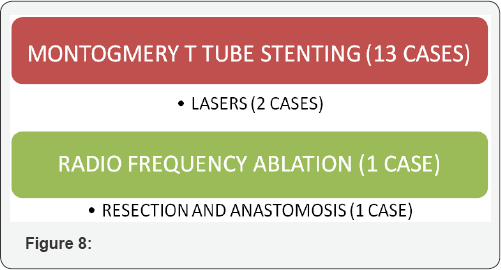
Depending on varied treatment options for LTS, each
having its own limitations, multiple modalities of management were
practiced owing to patient factors, surgeons factors, economic factors
etc (Figure 7). 17 cases were managed surgically by various modalities which are given below (Figure 8).
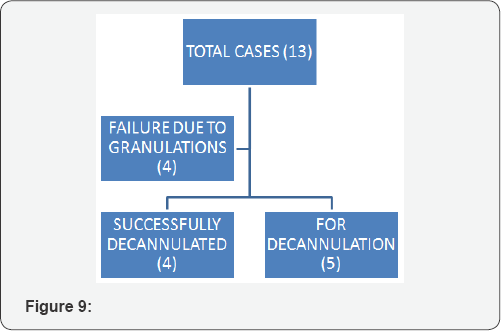
T-tube management is commonly practiced at our institute for varied reasons among which the results are as mentioned below (Figure 9) (Table 7).
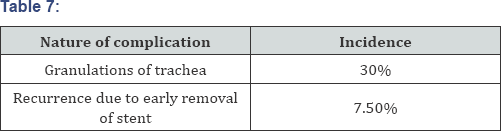
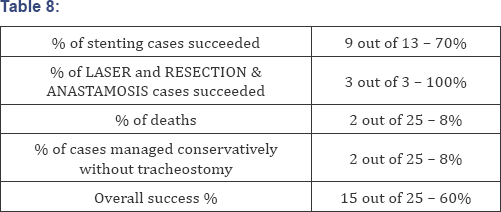
Granulations were the main problems in few cases
which might have been the result of infection, excessive movement of
tube against tracheal wall allergic reaction to stent They were noted
both above as well as below the tube. Overall percentages of results are
summarized below (Table 8).
In this current study, 25 cases of airway stenosis
with various etiologies have been observed. Tracheal stenosis should be
considered in the differential diagnosis of any patient who has recently
been in an intensive care unit and who presents with exertional
dyspnoea or monophonic wheeze, particular when it is unresponsive to
bronchodilators as already suggested in shahnazafrosa et al. [22].
In this study Male to female ratio was nearly 1:1. The gender influence
has been controversial in the literature. A predominance of female with
tracheal stenosis has been reported in two series by McCaffrey et al. [12]
and Mehta et al. respectively contradicting our statistics. Two out of
two cases of idiopathic stenosis in this study were females. Female
predominance is also reported in cases of idiopathic subglottic
stenosis. There were no apparent risk factors like diabetes, smoking,
alcoholism, chronic illness in any of the cases for development of these
lesions except for the striking etiological cause (post intubational/
post tracheostomy etc.) as already been mentioned in poetkar DM et al [23].
MacEwen first reported endotracheal intubation for anesthesia in 1880 [25].
Lindholm reported injuries to the larynx and trachea after intubation
in 1969.Patients usually remain asymptomatic until the trachea has
stenosed to 30% of its original diameter, and it may take as long as
three months before the diagnosis according to Spittle & McCluskey
et al. [25]
supporting this study where diagnosis after extubation ranged from 5
days to 1 year. All of our patients had severe (>50%) tracheal
stenosis with an average degree of stenosis of more than 70%. But the
incidence of Severe tracheal stenosis prevalence should be very low
especially since the introduction of large volume, low pressure
endotracheal tube cuffs, elimination of heavy ventilatory connecting
equipment, and meticulous care of the tracheostomy as suggested in the
article by Sajal & Sarmista de et al. [26]
A study by Norwood et al who followed 48 intubated patients for 30
months found that only 1 patient (2%) developed severe tracheal
stenosis, while mild to moderate stenosis was detected in 14 (29.3%)
patients. Our series reflects a large referral network and does not
necessarily reflect the true prevalence of the condition.
The site of the stenosis varies according to whether
the patient has had tracheostomy or only endotracheal intubation or
other etiology. Stenosis that developed as a web around an endotracheal
tube cuff is longer and more uniform than the stenosis around a tracheal
stoma where granulation tissue can extent from a fissure in the
anterior trachea or grow into a bulky granulomatous formation
surrounding a fracture cartilage [27].
On comparision tracheostomy induced stenoses were relatively lesser
than post intubational stenosess in our study i. e., 3:13 cases only One
particular case in this study showed development of tracheal stenosis
even after 2days of intubation, which can be supported by study of D R
Miller & G Sethi [18] in 1969 which shows development of tracheal lesion after 36 hours of intubation.
The determinant of treatment methods is whether
postintubation damage extends to tracheal cartilage or not. For now,
there is no accurate diagnostic study for viability of cartilage
preoperatively. In the literature, symptoms due to airway stenosis
occurred rapidly within one month in the case of patients with necrosis
of tracheal cartilage [28].
So it is concluded that the period between extubation and development
of symptoms is very informative in the management of post-intubation
tracheal stenosis.
All patients irrespective of mode of permanent
treatment assorted were maintained on steroids. Conservatively managed
cases which were under steroid cover had a non progressing lesion
thereafter as mentioned in Braidy et al. [29]-"
but the inflammatory nature of the lesion (as suggested by endoscopy
and radiology), the progressive deterioration in symptoms over one
month, and the rapid response to corticosteroids (five days) suggest a
therapeutic response to steroids”.
Most of our patients (13cases) underwent silicon T-tube stenting [30]
following stenotic segment release either by cold steel technique or
radiofrequency ablation followed by stenting with Montgomery T-tube of
which 9 cases (70%) are doing well. Rest of the four cases have suffered
from granulations following stenting. According to Cynthia et al the
occurrence of obstructing granulation tissue after stenting is reported
to be 12% to 28% in patients with benign disease and this study results
are correlating with it. One of the main drawbacks of these surgeries is
the risk of recurrence of tracheal stenosis due to granulation and
fibrotic tissue. Silicon tubes considered to be foreign bodies are
responsible for infections and granulations (as a reparative process or
due to bacterial infection) [31]. 4 out of 13 cases in this study developed granulations after stenting.
Both in vitro and in vivo, Mitomycin C have been
proven to be a potent inhibitor of human fibroblasts at concentrations
of 0.04mg/L. It has been used with some success in inhibiting the
vigorous granulation response noted after airway injury in animal models
and pediatrics [32].
Application of topical medications to shrink the granulation tissue can
be effective too. These medications may include steroids, which can be
applied directly to the tissue or injected just beneath the granulation
tissue. In addition, other medications decrease the number of fibroblast
cells, which help to create granulation tissue [33].
In 4 cases of stenting where granulations posed a problem, topical
mitomycin was used and 3 cases showed reduction in bulk of granulation
tissue along with post op steroid nebulisations.
Crusting and complete occlusion of T-tube is also
noted. Humidification of inspired oxygen, regular suctioning of both
limbs of the T-tube, and lavage with normal saline have been recommended
to prevent encrusting of the tube- Appadurai et al. [34].
Even in this study 2cases of tube blockage have been reported when
emergency removal of t tube had to be done . Apart from other modalities
of treatment, as considered by Puma et al. [35],
T tube stenting is one of the best alternatives. Silicon T tube
stenting is not just for primary management but can also be used to
support the reconstructed airway after laryngotracheal resections and
complex stenoses. But in this study all cases were stented as a part of
primary management only. Subjects on silicon tube were decanulated
between 12-24 months which is well between the span as suggested in
Fransesco and colleagues as 9-70 months [35].
In this current study 2 cases of glottic web were
managed by laser excision and keel placement for 6weeks are doing well
with 1year follow up without any recurrence similar to Benmansour et al.
[36]. Resection and an astamosis done in 1case is doing equally good without any recurrence.
Many papers and articles by Grillo, Mehta, Mccaaffrey
prove that open surgical techniques and the results of 1st stage
procedure are high relatively than a lesion undergoing repeated
interventions. As most of this study is inclined towards T tube,
discussion and comparisions are limited to it. "T-tubes are a
satisfactory alternative to tracheal resection and are preferred over
interbronchial stents for tracheal stenosis as T-tubes have decreased
rate of migration, allow for frequent irrigation and suctioning, are
easily removed in case of acute obstruction, and maintain a tracheostomy
stoma”-suggested by Julie M Schrader [37].
"The use of a T-tube in some patients with tracheal stenosis a very
good therapeutic method which should be used at present in indicated
cases” by Fiala P et al. [38]. Thus results of this study are well substantiated from these evidences.
Finally in the review of literature it is found that
"A bioresorbable stent that scaffolds the airway lumen and dissolves
after the remodeling process is completed has advantages over metallic
and silicone stents”. Kuoshungliu and colleagues designed and fabricated
a new mesh type bioresorbable stent with a backbone of polycaprolactone
(PCL), and evaluated its safety and biocompatibility in a rabbit
trachea model [39].
i. Post intubational airway stenosis - most common
cause. Shortest span of intubation-2 days ; longest span of
intubation-17days ; median span of intubation - 9 days.
ii. Post intubational stenosis;onset of symptoms. Earliest- 5days after extubation; maximum duration- 1year after extubation.
iii. As tracheostomy was commonest & earliest
intervention to save life,regaining normal sound production was common
desire of all the patients.
iv. T-tube stenting is the best and relatively cheaper mode of treatment for selective lesions.
v. Regular humidification & frequent suctioning
with NAHCO3 in initial stages may be required to prevent T-TUBE blockage
by dry crusting.
vi. T-Tube suctioning is practically difficult for the patient who got used to cleaning the inner tube of silver jackson's.
vii. All those cases which developed granulations after stenting were aged less than18years.
viii. Frequent follow ups of stenting cases by
Bronchoscopy in a public sector hospital with busy O.T is a bit
difficult job, so usage of a 70degree endoscope through stent has been
practiced.
ix. Application of topical mitomycin c for 6min after
excision of granulations by radiofrequency/electrocautery reduced the
incidence of granulations.
x. LASER- usage for this kind of cases is the best
alternate to prevent reccurence, but needs experienced practiotioner and
it is a costly procedure.
xi. RESECTION & ANASTAMOSIS is best procedure for selective lesions but only in hands of a well trained surgeon.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment