Parapharyngeal Space Tumors - "A Surgical Challenge"-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Parapharyngeal space tumors are rare entity. Overall
incidence is less than 0.5%. These tumors are divided into prestyloid
and post styloid tumors. Salivary gland neoplasma are common in
prestyloid compartment whereas Neurogenic tumors in post styloid
compartment. As these tumors are painless and does not express signs and
symptoms at early stage, diagnosis of such tumors needs critical
evaluation. Anatomic complexity of PPS makes surgical excision more
challenging. We have reported 4 cases of parapharyngeal space tumors
over a period of 10 years.
Background
Parapharyngeal space is an inverted pyramid from base
of the skull to hyoid bone. It is bounded medially by pharynx,
anteriorly pterygomandibular raphe, posterolaterally carotid sheath,
posteromedially retropharyngeal space, laterally above the level of
mandible it is bounded by ramus of mandible, deep lobe of parotid and
medial pterygoid muscle, below the level of mandible; it is bounded by
posterior belly of diagastric muscle. It is divided into prestyloid and
poststyloid compartment by aponeurosis of zuckercandle and testus [1]. 80% of the PPS tumours are benign while 20% are malignant [2]. Incidence of parapharyngeal space tumors is less than 0.5% [3].
Majority of the tumours are slow growing, painless and progressive in
nature. If untreated might result in severe life threatening
complications like airway obstruction and cranial nerve deficit
resulting in significant morbidity. Systematic diagnostic evaluation
plays an important role in diagnosis. Surgical excision has Pivotal
significance in PPS tumors. We have identified and reported four cases
of parapharyngeal space tumors at our centre over a period of 10 years.
Case 1
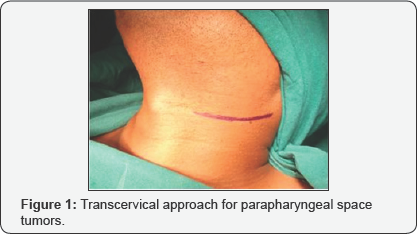
29 year old male presented with complain of painless
lateral neck swelling since 3 months. There was no history of dysphagia,
Hoarseness of voice. There was no cranial nerve involvement. FNAC
showed spindle cell tumor. On MRI there was 50x 37mm well circumscribed
lesion over left side of neck suggestive of schwannoma. Surgical
Excision of the tumor was done using transcervical approach (Figure 1).
There was no intra-operative complication. ICA, ECA, Vagus nerve and
IJV were identified and preserved. Tumor was excised completely (Figure 2).
Post operatively there was reduction in high pitch sounds. Origin of
tumor from vagus nerve was confirmed intra-operatively. Microscopic
picture revealed presence of mixed Antoni A and Antoni B cells
concluding to the microscopic features of schwannoma.
Case 2
34 year old female presented with painless swelling
over right side of neck. CT neck showed 64x46x35mm lesion in the carotid
space compressing right IJV and displacing it anterolaterally (Figure 3).
Superiorly it was extended up to carotid canal. Differential diagnosis
includes paraganglioma in view of intense enhancement of lesion and
vagal schwannoma in view of displacement pattern of vessel. FNAC was
suggestive of spindle cell tumor. Intraoperatively there was rupture of
internal carotid artery which was repaired with 6-0 ethilon, vagus nerve
was also sacrificed due to the severe adherence of the tumor to the
nerve.

Case 3
24 year old female complains of painless progressive
swelling with dysphagia to solids and liquids since 4yrs. CT scan showed
heterogeneously enhancing lesion 85x31mm with retrosternal extension
displacing major vessels laterally. Intraoperatively transcervical
incision was taken and tumor was dissected to free it from the major
vessels and nerves and it was removed in to (Figure 4).

Case 4
40 year female patient presented with swelling of left submandibular region since 1 month (Figure 5).
FNAC showed spindle cell tumor, USG showed 41x39mm Heterogenous mass
and left submandibular gland. CT Scan Showed 4.5cm enhancing well
circumscribed lesion, left submandibular gland and another 1.3x1cm
lesion adjacent to it. No dysphagia or hoarseness of voice,
intra-operatively Hypoglossal nerve was sacrificed. Lingual nerve was
identified and preserved. Histopathology report showed neurogenic tumour
i.e. schwannoma.

Discussion
Para-pharyngeal space (PPS) tumors are very rare. We
have identified 4 patients after reviewing 10 years retrospective data
of all head and neck tumors presented at Manavata curie cancer centre
Nashik. Incidence of parapharyngeal space tumors at our institute was
0.004%. Overall incidence of these tumors is less than 0.5%. These
tumors are slow growing, painless and patients express at later stage
when the size become considerably large. Usually patients are
asymptomatic but may exhibit dysphagia or hoarseness of voice. In our 4
patients only one patient had dysphagia to solids and liquids rest of
the patients were asymptomatic [4,5]. 80% of the tumors arising in this region are benign [2].
Pleomorphic adenoma is the most common tumor of prestyloid compartment
where poststyloid tumors are mostly neurogenic like shwannoma,
paraganglioma, neurofibroma, hemangiomas etc. Chordomas, lypomas,
lymphomas, chemodectomas, rhabdomyomas, chondrosarcomas, desmoid
tumours, ameloblastomas, amyloid tumours, ectomesenchymomas,
fibrosarcomas and plasmocytomas have also been reported [2].
Diagnosis of these tumors is difficult as they are
asymptomatic. Diagnostic evaluation constitutes CT scan and MRI to
clearly define the extent of the tumor mass. Arteriography also plays a
significant role to assess vascular compression. In our identified cases
CT scan was performed in 3 cases and MRI in one case. MRI has been
shown to gives better dimensions of the parapharyngeal space tumors.
Advantage of MRI is, it distinguishes tumor from Muscular structures and
give better dimentions of the tumor [6].
Arteriography was not performed in any of our cases.
Once the nonvascular nature of tumor is confirmed by radio-imaging, FNAC
can be performed for definitive diagnosis. FNAC is accurate in 90-95%
of the cases and helps in surgical planning [7]. Limited role is explained in post styloid compartment. We performed FNAC in all our patients and it was conclusive [8,9].
Schwannoma may arise at any age but in our institute
patient's age ranged from 3rd to 4th decades of life. There is no gender
predilection. Schwannoma may be of two types histologically consisting
of either Antoni A cells or Antoni B cells. We had two patients with
Antoni A cells and other one was of mixed variety [10].
Paragangliomas are tumors of autonomic nervous system. Head and neck
paragangliomas are unique in its variety as they don't release
catecholamines. Incidence of paraganglioma is 1 in 30,000 cases [11].
Histopathological picture shows two types of cells; Chief cells and
sustantecular cells. One of our patient's histological features were
identical to it.
Surgical management of parapharyngeal space tumors is
very challenging owing to anatomic complexity ofthe space and vicinity
of the tumor with major neurovascular structures. There are 7 different
approaches described for PFS tumors. Transcervical, Transcervical-
transparotid, Transoral-transcervical approach, Extended approach,
Transcervical-mandibulotomy aaproach, Transcervical-transmastoid
approach have been explained [12].
4cm is the limit for radical tumour excision with the transcervical
approach without mandibulotomy. For a safe and radical resection of
tumours > 4cm the “swing” approach or the transmandibular with a
double osteotomy is required [2].
We used transcervical approach without mandibulotomy in all cases.
Accesiblity was compromised in larger tumors but we could enucleate
entire tumor without much difficulty. ICA was ruptured in one case but
it was managed. Minimal accessibility may be a compromise but there is
less surgical morbidity and post op recovery is faster in our
experience.
Complications after surgical management are
unavoidable. Expected complications are due to sacrifice of cranial
nerves. There may be unexpected neurological complications in spite of
preservation of nerves like first bite syndrome, Trismus, facial nerve
weakness, orocutaneous fistula, Seroma. We experienced loss of high
pitched sounds in two of our patients and there was hypoglossal nerve
palsy as hypoglossal nerve was sacrificed in one case.
CT scan or MRI should always be performed in order to
distinguish prestyloid from poststyloid lesions and assessment of the
extension of the tumour and its relationship with adjacent structures.
Trans-cervical approach is safe and should be the first choice for large
tumors; other approaches are reserved for selected cases.
These are painless slow growing non malignant tumors
with very less incidence of recurrance. Management of PPS tumors is
challenging for surgeons. Neurological and Surgical complications should
always be explained to patients preoperatively. Preoperative assessment
and careful surgical manipulation are of utmost importance.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment