Non-Traumatic, Spontaneous Extra-Dural Haemorrhage: A Rare Neurosurgical Emergency of Beta-Thalassemia Major-Juniper Publishers
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
Non-Traumatic, Spontaneous Extra-Dural Haemorrhage: A Rare Neurosurgical Emergency of Beta-Thalassemia Major
Abstract
Intracranial Extradural Hematoma (EDH), a collection of blood between the skull and the dura, is a common sequelae of head trauma. Spontaneous EDH without underlying medical causes has been reported in intraspinal lesions but rarely in intracranial conditions. Spontaneous EDH with haematological disorders is rarer still. Previous literatures have reported on cases of spontaneous EDH because of sinus, middle ear, orbital infections, disorders of blood coagulation. We report a case of a spontaneous EDH on a background of Beta Thalassemia Major which has yet to be reported.
Keywords: Neurosurgery; Hematoma
Abbrevations: EDH: Intracranial Extradural Hematoma; GCS: Glasgow Coma Scale; CT: Computed Topography; MRI: Magnetic Resonance Imaging;
Introduction
Intracranial Extradural Hematoma (EDH), a collection of blood between the calvaria and the dura, is a common sequelae of head trauma, and can lead to significant morbidity and mortality if management is delayed [1]. Spontaneous EDH without underlying medical causes has been reported in intraspinal lesions but rarely in intracranial conditions [2,3]. Spontaneous EDH with haematological disorders is rarer still [4-6]. We report a case of a spontaneous EDH on a background of Beta Thalassemia Major. To the authors’ knowledge, this is the first reported case of spontaneous EDH with Beta Thalassemia Major, worldwide.
Case Report
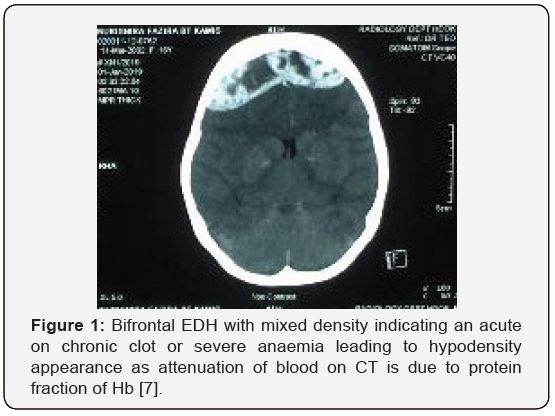
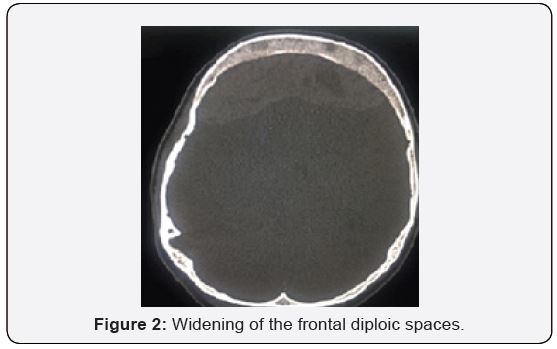
A transfusion-dependant, 16-year-old female with Beta Thalassemia Major complicated with Iron Overload (diagnosed at the age of 1 year and 4 months with HbA2 2.1% HbF 89.5%), presented to our casualty on the 31st of December 2018 after she was found unconscious at home by her parents. There was no history of head trauma or infection. Prior to presentation, she had complained of gradually worsening shortness of breath and headache over the course of 5 days. Upon neurological examination, her Glasgow Coma Scale (GCS) was E1V1M1 with unequal, bilaterally sluggish pupils. The right pupil was larger than the left. Vital signs were normal. She was markedly anaemic with a Haemoglobin concentration of 6.9g/dL. Coagulation profile results were not available due to technical issues. Other biochemistry parameters were within normal ranges. An urgent non-contrasted Computed Topography (CT) scan of the brain showed a thick bifrontal extradural hematoma of mixed densities with a maximum thickness of 2.3cm, causing mass effect to the surrounding brain parenchyma (Figure 1), and widening of the frontal and biparietal diploic spaces. (Figure 2) There were no skull fractures. Other history is significant for iron overload cardiomyopathy, proven on a previous Cardiac Magnetic Resonance Imaging (MRI) in 2015. An echocardiogram in the same year showed normal ventricular function. An emergent craniotomy and clot evacuation were done. Intraoperatively, there was no evidence of skull fracture. A thick, well-organised clot was seen bi-frontally. (Figure 3) Osteolytic and hemopoietic changes were seen over the anterior calvarium. (Figure 4) Slow diffuse bleeding was seen over the dura surface and osteolytic bone, which was controlled with bipolar cautery and application of bone wax.
Discussion
The aetiology of EDH is almost always traumatic [1]. Hematoma results from ruptured middle meningeal vessels or diploic veins, and skull fractures are estimated to be associated in 65-90% of patients [8]. Reported causes of spontaneous EDH include – vascular malformations of the dura, sinus, middle ear, or orbital infections, hematological disorders such as sickle cell anemia, Systemic Lupus Erythematosus (SLE), tumors, and open-heart surgery [9,10]. Spontaneous EDH associated with Thalassemia has never been reported in the literature to date, thus, the mechanism is vague. Hypercoagulability is a wellestablished characteristic of beta thalassemia, due to changes in lipid membrane composition of abnormal erythrocytes, with increased expression of negatively charged phosphatidylserine (PS) at the outer surface, constant platelet activation due to endothelial injury, and deficiency of natural anticoagulants. Thalassemic also have chronic low-grade inflammation and impaired fibrinolysis (Angchaisuksiri et al). These changes may account for the increased risk of thrombosis in these patients. Thrombosis is largely a subclinical process in Thalassemia, with autopsies finding microvascular platelet and fibrin thrombi [11]. We postulate that this may be the reason for chronic bone infarct. Other reports of spontaneous EDH in sickle cell anemia propose a similar mechanism of bone infarct, causing periosteal elevation, disruption of cortical bone, and eventually bleeding into the extradural place. However, the causative mechanism in sickle cell anemia is vaso-occlusion, not thrombosis [12]. Another postulation of spontaneous EDH is inadequate venous drainage causing venous hypertension and venous rupture. In hematological disorders, chronic extra-medullary hematopoiesis occurs. Hyper-proliferative bone marrow disrupts the inner and outer skull margins and precipitates extravasations of blood into the subgaleal and extradural spaces. In our case, the patient’s skull was found to have areas of blackish discoloration, pinpoint bleeding sites, and spongy bone, suggestive of skull infarction and hematopoietic bone (Figure 2). We hypothesize that the likely source of the EDH may be a combination of hyperproliferative bone with chronic infarcts. This theory may be confirmed with a histopathological examination of the bone. More research is required to support this hypothesis, which may not be possible due to the paucity of cases.
Conclusion
Non-traumatic spontaneous EDH should be considered in patients presenting with raised intracranial pressure symptoms, especially when significant co-morbidities are present. When diagnosed, urgent surgical decompression is indicated. The pathophysiology of EDH in haematological disorders is not well understood, and more research is required to understand this phenomenon. To our knowledge, this is the first case of spontaneous EDH associated with Beta-Thalassemia Major reported in the literature.
For more articles in Open access Journal of Head Neck & Spine Surgery | please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf

Comments
Post a Comment