Herniotomy Alone as Treatment for Scrotal Migration of Ventriculoperitoneal Shunt-Juniper Publishers
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
Herniotomy Alone as Treatment for Scrotal Migration of Ventriculoperitoneal Shunt
Abstract
Complication rate of ventriculoperitoneal (VP) shunt is from 11%-25%; differs from centre to centre. One of the rare complications of ventriculoperitoneal shunt is distal catheter migration into various abdominal contents including the scrotum. A few cases of scrotal migration of distal catheter have been reported in paediatric patients with different managements. Here we report a case of a 3-year-old child who presented with a right sided hydrocele with the distal end of the shunt in the left hemiscrotum 3 years following a VP shunt placement for congenital hydrocephalus. Herniotomy alone was our management in this case.
Keywords: Ventriculoperitoneal shunt; Scrotal migration Herniotomy
Introduction
Ventriculoperitoneal (VP) shunts are the most commonly performed operative procedures to treat hydrocephalus in children [1]. Shunt migration is one of the rare complications of VP shunt yet there are a few case reports have reported migration to the scrotum via patent Processus vaginalis due to the frequent incidence of shunt placement. In this article we report a rare case; the first out of 180 VPS done in the hospital; who presented with scrotal migration of VP shunt.
Case History
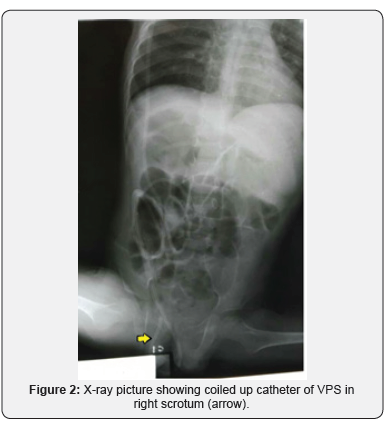
A 3-year-old boy presented with a swelling of the right inguino-scrotal region since a day prior. He had undergone right VP shunt procedure for congenital hydrocephalus at the age of 3months. The swelling was not associated with any complains of pain, fever or features of intestinal obstruction. On examination a gross swelling was noted in the right scrotal region (Figure 1). There were no clinical features of shunt malfunction. An X-ray of the abdomen and pelvis showed that the peritoneal end of the shunt coiled in the scrotum with its tip inside the abdomen (Figure 2). Patient asymptomatic of raised ICP and shunt block
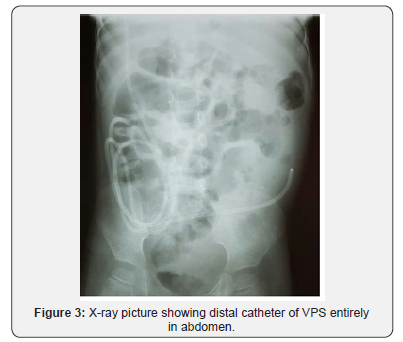
Patient was then planned for herniotomy. Prior incision, swelling could be reduced under general anaesthesia easily. Exploration was done subsequent revealed a thicken sac with empty contents and excised completely. VP shunt catheter was reduced with hernia sac preoperatively; the catheter was not visualized intraoperative. Post-operative X-ray confirmed the replaced entire distal shunt in abdomen (Figure 3). The patient is currently asymptomatic and doing well at follow-up.
Discussion
VP shunt insertion is a common treatment for hydrocephalus. The distal catheter of VP shunt can migrate into various body parts including the ventricle, scalp/subgaleal space, mouth, neck, breast, breast implant, thoracic cavity, pulmonary artery, intracardiac, lungs/pleural space/transdiaphragmatic, anterior chest wall, intraabdominal wall, abdominal subcutaneous fat tissue, umbilicus, stomach, large intestine, liver, gall bladder, bladder/urethra, inguinal sac, buttocks, canal of Nuck, which is the female counterpart of the spermatic cord, vulva/vagina, rectum/anus, and knee [3]. The reported incidence of distal migration of VP shunt is 10% [4]. But only less than 40 cases have been reported on scrotal migration of distal end of the shunt, as it is a rare phenomenon [5].
Normally, Processes vaginalis is patent at 60-70% of infants in first three months of life. It could be established as patent at 50-60% of 1-year olds and 40% for children between ages 2-16 years [6]. Increased abdominal pressure following shunt insertion may prevent obliteration of the Processus vaginalis and facilitates migration of the VP shunt into the scrotum [2]. Smaller size of peritoneal cavity in infancy compared with older children could be another etiologic factor for VP shunt migration to Processus vaginalis [7].
Scrotal migration of the distal VP shunt can lead to secondary hydrocoele, incarceration of catheter, and shunt malfunction, which in turn can cause worsening of the hydrocephalus [5]. A plain radiographic shunt series should be performed to assess integrity of VP shunt and plain computed tomography scan is needed to reassess the severity of hydrocephalus.
Management differs from case to case basis. The most common management encompassed shunt revision and herniotomy. Out of 36 cases reported 27 cases was managed with herniotomy and shunt revision and another 8 cases with shunt revision with no herniotomy done. Only 1 case was managed via herniotomy alone alike this case with manual compression of swollen scrotum [5].
For more articles in Open access Journal of Head Neck & Spine Surgery | please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf

Comments
Post a Comment