Extradural Epidermal Inclusion Cyst of Forehead: Case Report-Juniper Publishers
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
Extradural Epidermal Inclusion Cyst of Forehead: Case Report
Abstract
Epidermoid cysts occur when two epidermal surfaces fuse together during early intrauterine life and an ectodermal part is retained deep to the surface. They are very slow growing, and symptoms may not occur till middle age. Intradiploic epidermoid cysts are less common than the intradural varieties [1,2].
Keywords: Intradiploic epidermoid; Symptoms; Subcutaneous tissue; Epithelium
Abbrevations: FNAC: Fine Needle Aspiration Cytology; CT: Computed Tomography Scan; MRI: Magnetic Resonance Imaging
Case Report
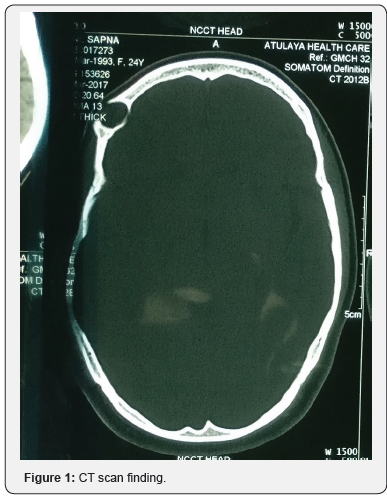
A 24-year-old female patient presented with right side forehead swelling since childhood which was insidious in onset, gradually progressive, persistent, not relieved with medication. On examination a single smooth ovoid cystic swelling of size 3×1cm was seen on right lateral part of forehead. Neurological examination was normal. Computed tomographic scan revealed a 32×27×14mm cystic lesion in right frontal bone with lysis of underlying bone. FNAC was suggestive of epidermal inclusion cyst. Surgery was performed. Horizontal skin incision given parallel to hairline. After dissecting subcutaneous tissue encapsulated cyst embedded in frontal bone was revealed. Cyst was thin walled and filled with pultaceous material. Frontal bone was drilled, cyst delineated all around. Under surface of cyst was found attached with dura with multiple small dehiscences of dural plate of around 0.5cm. Cyst along with its capsule removed enbloc and sent for histopathological examination. Surgical and gelfoam was used to fill the dural defect and remaining dead space was obliterated with gelfoam and drain no.10 was placed in the cavity for negative pressure. Drain was removed after 4 days and sutures were removed after 7 days.
Histological examination showed numerous keratin flakes and bits of stratified squamous epithelium suggestive of epidermal inclusion cyst. Patient was followed till six months without any complaints (Figures 1-3).
Discussion
Epidermoid cysts are lined by stratified squamous keratinized epithelium devoid of skin, appendages or glands. The etiopathogenesis of epidermoid cysts is debatable.
Inclusion of ectodermal tissue into the skull during embryogenesis is one main hypothesis. The other is secondary development of the lesion after inclusion of, migration of, or metaplasia to epidermal cells within the skull. Epidermoid cysts of the skull develop within the diploe. According to the Tessier classification, they arise along the trajectory of facial clefts in the frontal bone. Facial clefts follow the lines of facial prominence fusion. The location of epidermoid cysts along well-defined lines strongly supports inclusion of ecto-dermal cells during facial prominence fusion as the mechanism underlying epidermoid cyst development. Epidermoid cysts account for 1% of all intracranial tumors. Epidermoid cysts may arise secondary to trauma and may undergo malignant transformation [3]. Most patients belong to 20 to 60 years at diagnosis. The capsule is thin and the surface nodular and uneven. An epidermoid cyst of the frontal bone should be considered in all patients with pain or swelling of the supraorbital region, with or without exophthalmos or other ocular manifestations.
Late complications include development of a fistulous tract opening to the skin
a) Lateral to the eyebrow, discharging sinus infection, and meningeal manifestations.
b) CT shows an intradiploic sharply-defined lytic lesion and may disclose posterior extension or spread to the sinus or orbit. In differential diagnosis, malignancy must be ruled out. Other diagnoses include mucocele, granulomatous lesions, and connective-tissue tumors.
c) For frontal bone cysts, adequate exposure during surgery is essential to allow complete removal of the mass and capsule in order to prevent recurrences [4]. The eye-brow or coronal approach with frontal craniotomy ensures satisfactory exposure [5]. Long-term follow-up is needed given the risk of local recurrence.
Conclusion
Epidermoid cyst of the frontal bone is rare. Preoperative diagnosis is difficult, but CT and MRI images can suggest an epidermoid cyst, thereby helping to plan the surgical approach. Surgery is indispensable, and adequate exposure is required to allow complete excision and avoid recurrence.
For more articles in Open access Journal of Head Neck & Spine Surgery | Please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | Please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf

Comments
Post a Comment