Surgical Management for Non-Traumatic Syringomyelia using Syringo-Subarachnoid Shunt “T-Tube”: An Experience of 6 Cases-Juniper Publishers
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
Surgical Management for Non-Traumatic Syringomyelia using Syringo-Subarachnoid Shunt “T-Tube”: An Experience of 6 Cases
Authored by Ghassen Gader
Introduction
The natural history of syringomyelia is highly variable. In some cases, patients do improve or stabilize without surgery, while others deteriorate even with aggressive interventions. Various surgical procedures for the treatment of syringomyelia have been introduced, including posterior fossa decompression, syringostomy, syringoperitoneal shunting. But even though satisfactory results have been reported for most of these procedures, some authors have been critical of these techniques. Through this paper, we will try to make our contribution by reporting the results we have got after surgical management of 6 patients operated for syringomyelia by syringo-subarachnoid shunt using T-Tube.
Methods
Patients
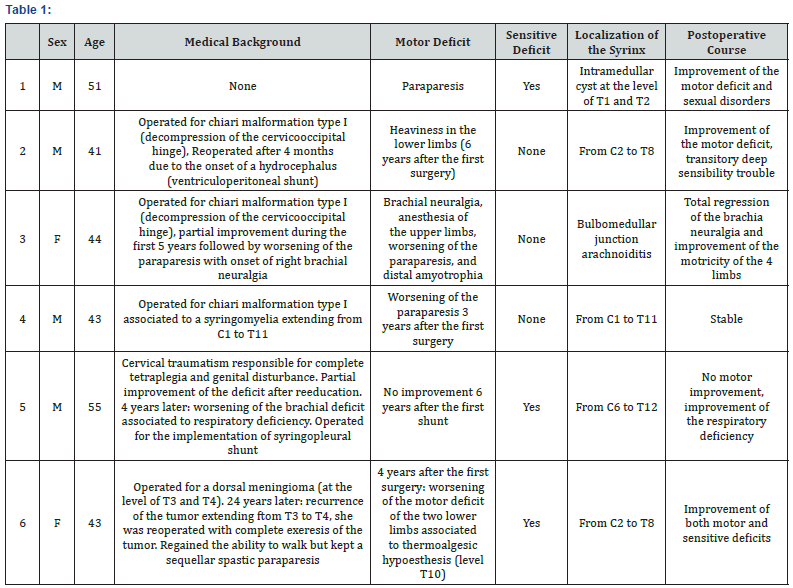
The mean age of our patients was 55.4 years. Etiologies of our patients’ syringomyelia are various: only one patient had post traumatic syringomyelia (6 years after trauma). One has an idiopathic intra medullar cyst; the four others were previously surgically managed: 3 for decompression of cervico-occipital hinge, and one for an intradural meningioma (Table 1). All patients had motor dysfunction, 4 had sensory disorders, and 3 had sexual or genital disturbances. About radiologic localizations of the syrinx, 4 patients had an intramedullar cavitation extending through cervical and dorsal medulla (Figure 1). 1 patient had bulbomedullary syringomyelia (Figure 2), and 1 had an intramedullary cyst localized in front of T1-T2 (Figure 3).

Surgical technique
The used technique for all our patients was a syringosubarachnoid shunt made through the implementation of a t-tube. Positioning was strict ventral. We proceed to a laminectomy followed by a durotomy in front of the widest portion of the intramedullary cavitation. The arachnoid is opened by making flecks, through which we carefully introduce the tip of the catheter at the level of the dorsal groove until the extraction of CSF out from the syrinx. Finally, the two arms of the T-catheter are attached to the arachnoid.
Follow up
Only one patient had transitory disturbances of the proprioceptive sensitivity, followed by a recover of the same anterior neurologic status. Two patients presented neither deterioration nor amelioration of motor or sensitive functions. The 3 other patients improved their preoperative status. This improvement concerned at most sensitive features. All our patients had postoperative MRI 6 months after surgery. This control imaging showed a radiologic improvement defined by a reduction of the size of the syrinx, found in 4 patients (Figure 4). Two patients had almost the same radiologic lesions as found on preoperative MRI.

Discussion
Syringomyelia is a known to be a disorder in which a cyst or cavitations are formed within the spinal cord. This abnormality called a syrinx can expand and elongate over time, destroying the spinal cord [1]. Syringomyelia is associated with numerous different pathologies, including spinal trauma, craniocervical anomalies mainly chiari malformations, meningitis, spinal tumor [2]. The pathogenesis of syringomyelia is still a subject of controversies. The most commonly accepted theory is that the spinal cord’s cavitation occurs when CSF is forced to get through the fourth ventricle into the central canal. This may be the consequence of either a caudally directed pulse wave, or a pressure gradient at the level of the foramen magnum [3]. Physiopathological theories has conditioned therapeutic approaches for syringomyelia and led to the development of several operative procedures depending on its supposed etiology and pathogenesis [4]. Posterior fossa decompression [5], syringoperitoneal shunt [6], syringopleural shunt [7], myelotomy coupled with lumboperitoneal shunt [8], syringosubarachnoid shunt [9], and several other techniques, have all been described with varying success.
Several ancient reports have been considering that the results of syringo-subarachnoid shunt as disappointing. Among their arguments to explain this failure were discussed the difficulty of manipulation of the T-tube with a high risk of medullar lesion [6,10], and the frequency of shunt obstruction as a result of the collapse of the syrinx cavity around the shunt tip [4,11]. This failure was mainly discussed in post-traumatic syringomyelia, where spinal injury produces numerous abnormalities, such as subarachnoid adhesions, spinal deformity or stenosis in addition to the syrinx, limiting the efficiency of any shunting procedure [12].
The new surgical techniques of implantation of T-Tube have managed to break out with the anterior shortages [6,10]. In our new shunting procedure, we inserted just one arm of the T-tube into the syrinx cavity and located the other arm outside the cord, in the sub-arachnoid space. Thus, we can protect the cord from tube rotation, but also have the possibility to easily remove the tube when necessary, without prejudice on the cord. Also, we could easily anchor the tube to the dura, and thus prevent migration resulting in shunt malfunction.
According to several authors [13], the most important factor in the occlusion of the shunt system is the development of arachnoiditis and adhesions of the arachnoid around tip of the shunt tubing. Anatomically [9], the dorsal and ventral spinal subarachnoid spaces are different. Many trabeculae exist between the pia mater of the dorsal cord surface and the dorsal arachnoid membrane; however, there are no arachnoid trabeculae on the ventral surface. Using the standard technique for syringosubarachnoid shunting, the dorsal subarachnoid space is the usual site for distal catheter placement and the anatomy of this space may contribute to delayed shunt malfunction. In the modified technique described here, the shunt is inserted into the syrinx at the dorsal root entry zone and the distal tip is inserted into the anterolateral subarachnoid space.
The results of our series support the reports claiming the interest of T-Tube shunt technique. Clinically, 50% of the cases of our series improved their preoperative status, and 50% kept the same signs without postoperative worsening. 66% had radiological improvement with regression of the syrinx; the others had the same preoperative aspects with no worsening.
We do think that with further technical refinement, we could reach better clinical and radiological results.
Conclusion
According to our good results, this new technique seems to be promising in the treatment of non-traumatic syringomyelia. For post-traumatic syringomyelia, an associated broad release of subarachnoid spaces is required. The study of a larger series is necessary in order to a better evaluation of the effectiveness of this technique.
For more articles in Open access Journal of Head Neck & Spine Surgery | please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf

Comments
Post a Comment