Postsurgical Complications after Spine Surgery-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
We present a case of a 22-month-old infant who
undergoes a surgical procedure consisting of performing cervical
arthrodesis after placement of a halo of cervical traction and thoracic
harness. The patient presented an alteration in the formation and
segmentation of the cervico-dorsal vertebral bodies, alteration of the
vertebral canal and angulation of the medullary cord. In the
postoperative period, the main complications are intense pain that
requires intensification of sedo analgesia, sepsis, diaphragmatic
paralysis secondary to surgery, and respiratory and hepatic failure due
to chest compression of the harness.
Keywords: Vertebral malformation Pain Cervical halo Thoracic harness Respiratory failure Liver failure
Abbrevations: ICU: Intensive Care Unit; CT: Computed Tomography
The malformations of the spine are a group of
polymorphic anomalies, from small asymptomatic lesions to important
disorders responsible for vertebral deformities, neurological disorders
and even respiratory failure. The orthopedic and neurosurgical treatment
depends on the severity of the clinical affectation [1,2].
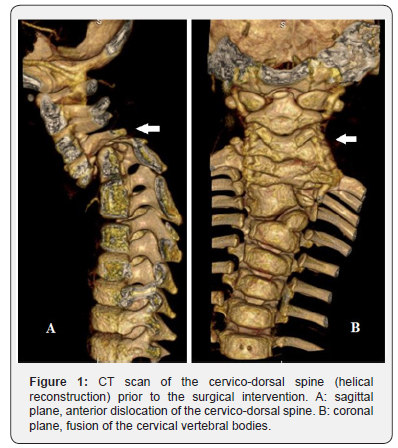
Infant of 22 months with antecedent of alteration in
the formation and segmentation of the cervico-dorsal vertebral bodies,
alteration of the vertebral canal and angulation of the medullary cord
(Figure 1), in follow-up by Rehabilitation and Neurosurgery. She starts
at 21 months right brachial palsy, so added to the degree of spinal
angulation is indicated neurosurgical intervention consisting of
placement of a halo of cervical traction and vertebral arthrodesis in a
second time. Enter the pediatric Intensive Care Unit (ICU) after
placement of the cervical halo and thoracic harness for adaptation and
initial management of pain with sedation. She arrives without invasive
ventilation and with spontaneous movements of the four extremities. 24
hours after admission, she presents episodes of desaturation, cyanosis
and gasping, with severe respiratory acidosis, which requires
orotracheal intubation and connection to invasive mechanical
ventilation. Chest x-ray and urgent cranial Computed Tomography (TC)
were performed without evidence of postoperative complications. The
cervical halo is removed, and
the thoracic harness is loosened, presenting frank improvement of
ventilation in the following hours. 48 hours after the episode, cervical
halo is repositioned, thoracic harness is removed and cervical traction
with weight is placed. In the following days, it is necessary to
intensify sedo analgesia due to pain. 9 days after admission to the ICU,
the surgical intervention was completed by performing vertebral
corpectomy with cervical arthrodesis. He returns to the ICU having
removed cervical traction with weight, repositioning the thoracic
harness and maintaining a cervical halo. Progressive descent of the
respiratory support is performed, invasive ventilation being removed 48
hours after the arthrodesis. Subsequently, she tends to hypercapnia and
respiratory acidosis. Non-invasive ventilatory support is started,
without improvement. Given the suspicion of restrictive etiology due to
external thoracic compression, the thoracic harness is loosened,
improving thoracic expansion and ventilation. 14 days of admission, she
presents hypotension, tachycardia, coagulopathy and fever, which
required several volume loads with crystalloids and administration of
dopamine in continuous perfusion. Sepsis is suspected, so treatment with
meropenem and vancomycin is initiated. In this context, she requires
again connect to invasive ventilation due to respiratory failure. 48
hours after the onset of the sepsis, she presents acute liver failure of
probable ischemic origin (ALT/LDH ratio <1.5) in the context of
hyper transaminasemia (AST 13246 U/L, ALT 5668 U/L), coagulopathy and
hepatomegaly. Given the suspicionof mechanical compromise by the
harness, it is immediately
removed, and the treatment is adjusted by removing the
drugs with hepatic metabolism. Treatment of acute liver
failure is initiated, adding treatment with carbaglumic acid to
hyperammonemia, N-acetylcysteine and liposomal amphotericin
B as prophylaxis. She begins progressive improvement of hepatic
insufficiency and septic shock by suspending dopamine support
4 days after, allowing a decrease in respiratory support and
sedo analgesia. Germs are not isolated in the collected blood
cultures. 9 days after the septic shock, cervical halo and invasive
mechanical ventilation are removed.
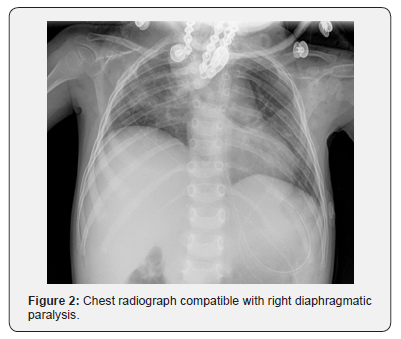
She presents again respiratory failure and right
diaphragmatic paralysis secondary to surgery is suspected,
which is confirmed by radiological and neurophysiological
study (Figure 2). In the following weeks she presents a torpid
evolution. She tends to hypertension in the context of withdrawal
syndrome and requires an increase in sedo analgesia. In view
of the difficulty in permanently removing invasive mechanical
ventilation associated with the presence of a justifiable cause of
respiratory failure and being a patient with difficult intubation,
a tracheostomy was performed. The intermittent disconnection
of the respirator begins in the following weeks. It is possible
to normalize the blood pressure and resolve the withdrawal
syndrome. During the evolution she presents difficulties in the
tolerance of the enteral nutrition and in the oral intake, deciding
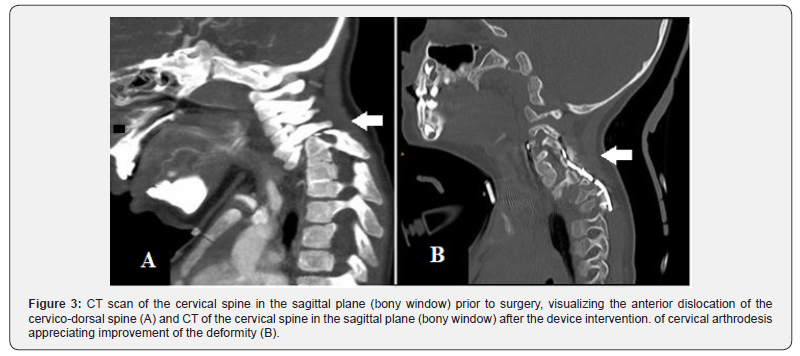
to perform a gastrostomy. CT of the cervical spine performed
one month after the intervention shows an improvement in the
vertebral malformation (Figure 3).
Discussion
Malformations of the spine require management by a
multidisciplinary team. Early diagnosis allows early initiation
of rehabilitative and orthopedic treatment in those cases that
require it. Depending on the type, they can cause scoliosis
and / or developmental congenital kyphosis and surgical
treatment is required the first years of life [1]. In this case, the
neurosurgical indication is posed after the onset of brachial
palsy in addition to the vital risk due to spinal cord angulation.
During the postoperative period, the main complications are
pain management and withdrawal syndrome, a septic shock,
respiratory and liver failure, secondary to chest compression
due to the harness and diaphragmatic paralysis secondary to
surgery. The episode of severe respiratory acidosis that appears
24 hours after admission is considered due to carbon dioxide
intoxication due to hypercapnia secondary to hypoventilation
due to the thoracic harness.
The ischemic liver failure is a rare cause of acute liver failure
both in childhood and in adults. The etiopathogenesis involves
low cardiac output secondary to postoperative cardiovascular
surgery, sepsis and extrinsic abdominal compression [3]. In this
case, it is believed that low cardiac output is involved due to the
septic pattern and the decrease in hepatic blood flow secondary
to compression by the thoracic harness. From the histological
point of view, ischemic hepatitis is characterized by originating
centrilobular necrosis with absence of inflammatory elements
[4]. At the analytical level, it is characterized by a marked and
reversible elevation of the transaminases and the LDH enzyme
with an ALT/LDH ratio lower than 1.5. The treatment of
ischemic hepatitis includes the management of the underlying
cause and supportive treatment of liver failure. It tends to
resolve quickly after the improvement of the underlying cause.
However, delay in diagnosis implies worse results [5]. In this
case, the transaminases fell quickly, reducing to a quarter after
48 hours of withdrawing the thoracic harness and normalizing
after 15 days. Another of the main postoperative complications
was diaphragmatic paralysis, which although infrequent, can
trigger an important respiratory compromise. It should be
suspected especially in the postoperative period of thoracic
and cardiac surgery when there is unexplained difficulty todecrease the respiratory assistance or after a failed extubation.
The chest radiograph shows a marked elevation of the affected
hemidiaphragm. The ultrasound allows a dynamic study of the
diaphragm and determines if there is absence or decrease in
diaphragmatic mobility. Electromyography allows to evaluate
the phrenic nerve and the diaphragm. The treatment can be
conservative, based on respiratory rehabilitation, or surgical.
There is not consensus as to which is the most appropriate [6,7].
Several of the postsurgical complications presented by the
patient were secondary to the use of the thoracic harness. It is a
mechanical device used to optimize the traction function of the
cervical halo. However, due to the mechanism, it compromises
respiratory and circulatory function, especially in pediatric
patients. The presented case is considered instructive since there
was no experience on the use of this device in children. For this
reason, it is essential for future cases to know the complications
due to the use of this type of device.
Juniper publishers-Journal of Head Neck
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment