Non-Traumatic, Spontaneous Extra-Dural Haemorrhage: A Rare Neurosurgical Emergency of Beta-Thalassemia Major-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Intracranial Extradural Hematoma (EDH), a collection
of blood between the skull and the dura, is a common sequelae of head
trauma. Spontaneous EDH without underlying medical causes has been
reported in intraspinal lesions but rarely in intracranial conditions.
Spontaneous EDH with haematological disorders is rarer still. Previous
literatures have reported on cases of spontaneous EDH because of sinus,
middle ear, orbital infections, disorders of blood coagulation. We
report a case of a spontaneous EDH on a background of Beta Thalassemia
Major which has yet to be reported.
Keywords: Neurosurgery; Hematoma
Abbrevations: EDH: Intracranial Extradural Hematoma; GCS: Glasgow Coma Scale; CT: Computed Topography; MRI: Magnetic Resonance Imaging;
Intracranial Extradural Hematoma (EDH), a collection
of blood between the calvaria and the dura, is a common sequelae of head
trauma, and can lead to significant morbidity and mortality if
management is delayed [1]. Spontaneous EDH without underlying medical
causes has been reported in intraspinal lesions but rarely in
intracranial conditions [2,3]. Spontaneous EDH with haematological
disorders is rarer still [4-6]. We report a case of a spontaneous EDH on
a background of Beta Thalassemia Major. To the authors’ knowledge, this
is the first reported case of spontaneous EDH with Beta Thalassemia
Major, worldwide.
A transfusion-dependant, 16-year-old female with Beta
Thalassemia Major complicated with Iron Overload (diagnosed at the age
of 1 year and 4 months with HbA2 2.1% HbF 89.5%), presented to our
casualty on the 31st of December 2018 after she was found unconscious at
home by her parents. There was no history of head trauma or infection.
Prior to presentation, she had complained of gradually worsening
shortness of breath and headache over the course of 5 days. Upon
neurological
examination, her Glasgow Coma Scale (GCS) was E1V1M1 with unequal,
bilaterally sluggish pupils. The right pupil was larger than the left.
Vital signs were normal. She was markedly anaemic with a Haemoglobin
concentration of 6.9g/dL. Coagulation profile results were not available
due to technical issues. Other biochemistry parameters were within
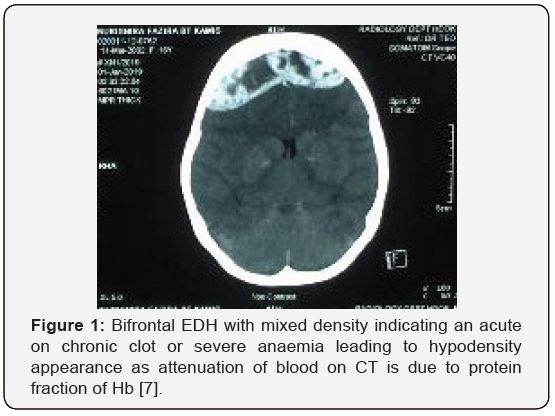
normal ranges. An urgent non-contrasted Computed Topography (CT) scan of
the brain showed a thick bifrontal extradural hematoma of mixed
densities with a maximum thickness of 2.3cm, causing mass effect to the
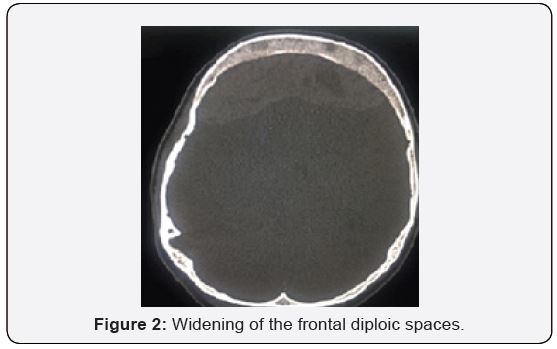
surrounding brain parenchyma (Figure 1), and widening of the frontal and
biparietal diploic spaces. (Figure 2) There were no skull fractures.
Other history is significant for iron overload cardiomyopathy, proven on
a previous Cardiac Magnetic Resonance Imaging (MRI) in 2015. An
echocardiogram in the same year showed normal ventricular function. An
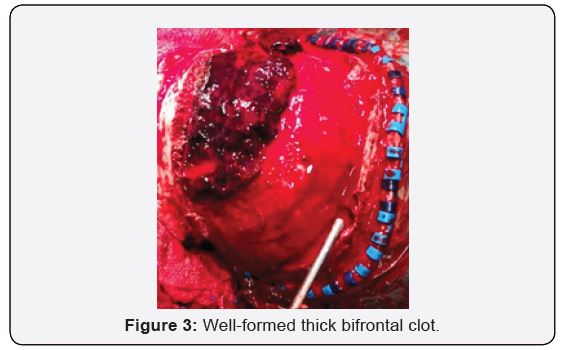
emergent craniotomy and clot evacuation were done. Intraoperatively,
there was no evidence of skull fracture. A thick, well-organised clot
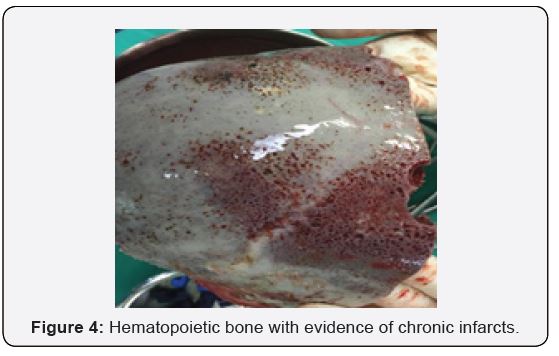
was seen bi-frontally. (Figure 3) Osteolytic and hemopoietic changes
were seen over the anterior calvarium. (Figure 4) Slow diffuse bleeding
was seen over the dura surface and osteolytic bone, which was controlled
with bipolar cautery and application of bone wax.
Discussion
The aetiology of EDH is almost always traumatic [1].
Hematoma results from ruptured middle meningeal vessels or
diploic veins, and skull fractures are estimated to be associated
in 65-90% of patients [8]. Reported causes of spontaneous EDH
include – vascular malformations of the dura, sinus, middle ear,
or orbital infections, hematological disorders such as sickle
cell anemia, Systemic Lupus Erythematosus (SLE), tumors, and
open-heart surgery [9,10]. Spontaneous EDH associated with
Thalassemia has never been reported in the literature to date,
thus, the mechanism is vague. Hypercoagulability is a wellestablished
characteristic of beta thalassemia, due to changes
in lipid membrane composition of abnormal erythrocytes, with
increased expression of negatively charged phosphatidylserine
(PS) at the outer surface, constant platelet activation due to
endothelial injury, and deficiency of natural anticoagulants.
Thalassemic also have chronic low-grade inflammation and
impaired fibrinolysis (Angchaisuksiri et al). These changes may
account for the increased risk of thrombosis in these patients.
Thrombosis is largely a subclinical process in Thalassemia, with
autopsies finding microvascular platelet and fibrin thrombi
[11]. We postulate that this may be the reason for chronic bone
infarct. Other reports of spontaneous EDH in sickle cell anemia
propose a similar mechanism of bone infarct, causing periosteal
elevation, disruption of cortical bone, and eventually bleeding
into the extradural place. However, the causative mechanism
in sickle cell anemia is vaso-occlusion, not thrombosis [12].
Another postulation of spontaneous EDH is inadequate venous
drainage causing venous hypertension and venous rupture. In
hematological disorders, chronic extra-medullary hematopoiesis
occurs. Hyper-proliferative bone marrow disrupts the inner and
outer skull margins and precipitates extravasations of blood into
the subgaleal and extradural spaces. In our case, the patient’s
skull was found to have areas of blackish discoloration, pinpoint
bleeding sites, and spongy bone, suggestive of skull infarction and
hematopoietic bone (Figure 2). We hypothesize that the likely
source of the EDH may be a combination of hyperproliferative
bone with chronic infarcts. This theory may be confirmed with
a histopathological examination of the bone. More research is
required to support this hypothesis, which may not be possible
due to the paucity of cases.
Non-traumatic spontaneous EDH should be considered in
patients presenting with raised intracranial pressure symptoms,
especially when significant co-morbidities are present. When
diagnosed, urgent surgical decompression is indicated. The
pathophysiology of EDH in haematological disorders is not
well understood, and more research is required to understand
this phenomenon. To our knowledge, this is the first case of
spontaneous EDH associated with Beta-Thalassemia Major
reported in the literature.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment