Neck Radiotherapy Increases the Risk of Syncope During Awake Airway Management: A Report of Two Cases-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Radiotherapy for head and neck cancer may causes
baroreflex dysfunction and can lead to syncope. Syncope is usually a
benign clinical condition and self-limit. However, in patients with
difficult airway their spontaneous recovery can be interrupted by the
significant hypoxia caused by airway obstruction. This might lead to
situation of cannot intubate and cannot oxygenate requiring emergency
surgical airway. Here we report two cases in which previous radiotherapy
treated patients developed syncope during preparation for awake
intubation resulting in emergency surgical access.
Keywords: Airway Syncope Neck radiotherapy Awake airway management
Abbrevations:
TLOC: Transient Loss of Consciousness; NRT: Radiotherapy to The Neck;
BP: Blood Pressure; HR: Heart Rate; CICO: Cannot Intubate, Cannot
Oxygenate; OR: Operating Room; BPM: Beats Per Minute; ETT: Endotracheal
Tube; SCC: Squamous Cell Carcinoma; IV: Intravenous; LMA: Laryngeal Mask
Airway
Introduction
Syncope is defined as Transient Loss of Consciousness
(TLOC) owning to brain hypoperfusion. It is characterized by quick
onset, short duration and is self-limited. It is generally a benign
clinical condition and has a reported overall mortality rate of 0.28%
from all causes [1]. Clinical reports have shown that Radiotherapy to
The Neck (NRT) for cancer treatment causes impairment of the baroreflex
response and results in baroreflex dysfunction. Studies have also
demonstrated a positive correlation between NRT and syncope [2,3].
Although full compensation for baroreflex dysfunction may be achieved in
daily life, these individuals may have a decreased tolerance to
emotional or physical distress resulting in exacerbated Blood Pressure
(BP) and Heart Rate (HR) changes with stimulation. We report two cases
in which patients developed TLOC during airway preparation for awake
intubation, resulting in the situation of “Cannot Intubate, Cannot
Oxygenate (CICO)”, and their airways were managed by emergency surgical
access.
Case 1
62-year-old, 78kg female with a past medical history
of controlled chronic hypertension and recurrent tongue cancer presented
for direct laryngoscopy, tongue biopsy and possible tracheostomy. The
patient underwent a partial glossectomy 13months previously due to
primary oral tongue cancer followed by bilateral neck radiotherapy.
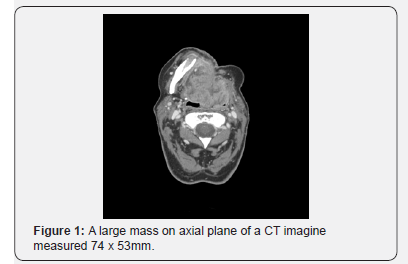
Tumor assessment revealed a large mass extending from the right base of
the tongue to the ipsilateral vallecular region, (Figure 1) but no
hypopharyngeal or laryngeal airway obstruction. Awake flexible scope
intubation via nasal approach was planned. Upon arrival Operating Room
(OR), the patient was placed on the OR table with the head elevated 30
degrees. Her first BP, HR and room air O2 saturation readings in the OR
were 165/82mmHg, 71 beats per minute (bpm) and 100%, respectively. She
received 2mg midazolam and 50mcg fentanyl intravenously upon arrival to
the OR. Attempted placement of a # 28 nasal trumpet into the nares for
dilation purposes caused significant discomfort as the result
Case 2
58-year-old female with a medical history of well-controlled
chronic hypertension and right vocal fold recurrent Squamous
Cell Carcinoma (SCC) presented for a total laryngectomy. Her
primary laryngeal cancer was treated with bilateral neck
radiotherapy two years prior to the surgery. Patient denied any
history of cardiovascular disease. She presented with a weak
and hoarse voice, but no difficulty breathing. She had a BMI of
38kg/m2 and neck circumference of 39cm. Airway assessment
revealed a Mallampati 3 airway without significant abnormality
in any other routine airway assessments. Video laryngoscopy
performed one week prior to surgery revealed an exophytic
tumor growing on her right vocal cord with immobilization
of the ipsilateral true vocal folder. However, the airway was
unobstructed. Based on the above findings, an awake flexible
scope intubation was planned. The patient had a baseline BP,
HR, and oxygen saturation of 148/72mmHg, 82 bpm and 98%
on room air, respectively. In the OR, the patient was placed in
the siting position with 2 L/min of O2 through a nasal cannula.
While placing monitors, the patient became pale and then
became unresponsive. The pulse oxygen waveform showed pulserate of 30s bpm with weak pulse by palpation, but her BP could
not be obtained by sphygmomanometer. Ephedrine (15mg)
was immediately administered Intravenously (IV) followed by
200mcg of phenylephrine. Despite the efforts of mask ventilation
with 100% oxygen, her O2 saturation continued falling. Trismus
was also evident when attempting insertion of an oral airway.
Subsequently, a Laryngeal Mask Airway (LMA) was placed
after intravenous administration of 120mg succinylcholine, but
no improvement of oxygenation was achieved. An emergent
tracheostomy was performed at O2 saturation in the low 80s%
by the surgeon. Thereafter, the patient was allowed to regain
consciousness and exhibited a normal neurologic assessment.
Surgery was then continued and completed in three hours.
Postop 12 leads EKG showed a normal sinus rhythm with HR of
68 bpm. The cardiology consult suspected a vasovagal syncope
as the cause of TOLC. No further evaluation was performed. In
PACU visit, patient had no recollection of the intraoperative
events. She underwent an uneventful hospitalization and was
discharged from the hospital on post-operative day #5.
Discussion
The sequential events developed in the two cases resembled
a cycle of reflex syncope. In these two cases, previous NRT
predisposed patients to potential baroreflex dysfunction.
Emotional distress and/or additional painful stimulation played
an important role in triggering the hemodynamic instability by
exacerbated BP and HR changes resulting in TLOC. However, the
self-recovery was interrupted by significant hypoxia caused by
airway obstruction. Without quickly establishing invasive airway
access, both cases may have resulted in significant patient
morbidity.
In patients with reflex syncope, stimulation from the
circulatory and visceral receptors to the brain via the
corresponding somatic sensory pathway, glossopharyngeal or
valgus nerves, strong emotional distress may directly activate or
facilitate activation of this reflex. The efferent paths consist of
the valgus nerve to heart and sympathetic fibers to the heart and
vessels. The degrees of vasodepressor and bradycardia, or both,
result in varying levels of manifestations. Most syncope attacks
occur in the upright posture reflecting the mechanism of central
hypovolemia in loss of consciousness and memory dysfunction
during an attack [4]. In a healthy individual, the functional
integrity of baroreflex plays a protective role in preventing
syncope. Impaired baroreflex is a mechanism resulting in
inability of sympathetic response to systemic hypotension [5,6].
A previous study demonstrated that impaired baroreflex predicts
the development of syncope during tilted test [7].
Baroreflex failure resulting from NRT is a rare clinical
entity. However, radiotherapy-induced baroreflex dysfunction
is common. Lack of heart rate and blood pressure response to
valsalva maneuverer and vasoactive challenging tests in patients
undergone NRT were found in all the patients in the study [8,9];and decreasing hemodynamic responses to surgical stimulations
in patients with NRT undergoing general anesthesia was also
reported [10]. Therefore, the patients with full compensation
of dysfunctional baroreflex in their daily life may develop
baroreflex decompensation under certain circumstances (the
triggers) resulting in loss of hemodynamic autoregulation and
episode of syncope.
Despite detrimental effects of TLOC developing at critical
moments, a routine test of baroreflex function in asymptomatic
patients is not practical. Therefore, carefully inquiry into
the history of fainting or near fainting in patients who have
undergone NRT is important to recognize the patients with
increased risk of syncope. During airway management,
emotional distress and anxiety should be controlled before the
onset of an awake intubation procedure. Every effort should be
made to prevent central hypoperfusion resulting in TLOC and
collapse of airway by avoiding prolonged erect position and
promptly treating hypotension and bradycardia. To manage a
difficult airway, one must be aware that repeated stimulation
of the glossopharyngeal nerve distribution (posterior 1/3 of
tongue) by airway instrumentation may worsen the symptoms
and prolong the recovery period; therefore, the benefits versus
the risk ratio of technique chosen to manage the airway must be
carefully considered. Nevertheless, managing a difficult airway
with a concurrent sudden onset event is challenging. Prevention
and early treatment are key to success and the avoidance of
catastrophic results.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment