Extradural Epidermal Inclusion Cyst of Forehead: Case Report-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Epidermoid cysts occur when two epidermal surfaces
fuse together during early intrauterine life and an ectodermal part is
retained deep to the surface. They are very slow growing, and symptoms
may not occur till middle age. Intradiploic epidermoid cysts are less
common than the intradural varieties [1,2].
Keywords: Intradiploic epidermoid; Symptoms; Subcutaneous tissue; Epithelium
Abbrevations: FNAC: Fine Needle Aspiration Cytology; CT: Computed Tomography Scan; MRI: Magnetic Resonance Imaging
A 24-year-old female patient presented with right
side forehead swelling since childhood which was insidious in onset,
gradually progressive, persistent, not relieved with medication. On
examination a single smooth ovoid cystic swelling of size 3×1cm was seen
on right lateral part of forehead. Neurological examination was normal.
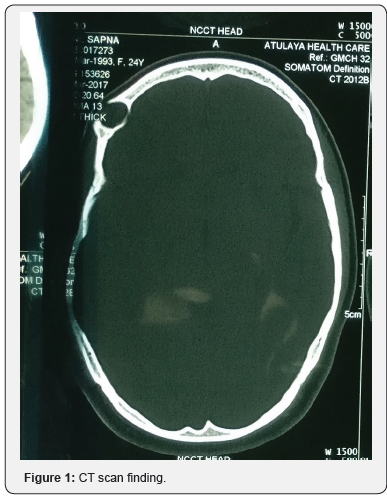
Computed tomographic scan revealed a 32×27×14mm cystic lesion in right
frontal bone with lysis of underlying bone. FNAC was suggestive of
epidermal inclusion cyst. Surgery was performed. Horizontal skin
incision given parallel to hairline. After dissecting subcutaneous
tissue encapsulated cyst embedded in frontal bone was revealed. Cyst was
thin walled and filled with pultaceous material. Frontal bone was
drilled, cyst delineated all around. Under surface of cyst was found
attached with dura with multiple small dehiscences of dural plate of
around 0.5cm. Cyst along with its capsule removed enbloc and sent for
histopathological examination. Surgical and gelfoam was used to fill the
dural defect and remaining dead space was obliterated with gelfoam and
drain no.10 was placed in the cavity for negative pressure. Drain was
removed after 4 days and sutures were removed after 7 days.
Histological examination showed numerous keratin
flakes and bits of stratified squamous epithelium suggestive of
epidermal inclusion cyst. Patient was followed till six months without
any complaints (Figures 1-3).


Discussion
Epidermoid cysts are lined by stratified squamous
keratinized epithelium devoid of skin, appendages or glands. The
etiopathogenesis of epidermoid cysts is debatable.
Inclusion of ectodermal tissue into the skull during
embryogenesis is one main hypothesis. The other is secondary
development of the lesion after inclusion of, migration of, or
metaplasia to epidermal cells within the skull. Epidermoid cysts
of the skull develop within the diploe. According to the Tessier
classification, they arise along the trajectory of facial clefts in the
frontal bone. Facial clefts follow the lines of facial prominence
fusion. The location of epidermoid cysts along well-defined lines
strongly supports inclusion of ecto-dermal cells during facial
prominence fusion as the mechanism underlying epidermoid cyst
development. Epidermoid cysts account for 1% of all intracranial
tumors. Epidermoid cysts may arise secondary to trauma and may
undergo malignant transformation [3]. Most patients belong to
20 to 60 years at diagnosis. The capsule is thin and the surface
nodular and uneven. An epidermoid cyst of the frontal bone
should be considered in all patients with pain or swelling of the
supraorbital region, with or without exophthalmos or other ocular
manifestations.
Late complications include development of a fistulous tract
opening to the skin
a) Lateral to the eyebrow, discharging sinus infection, and
meningeal manifestations.
b) CT shows an intradiploic sharply-defined lytic lesion
and may disclose posterior extension or spread to the sinus or
orbit. In differential diagnosis, malignancy must be ruled out.
Other diagnoses include mucocele, granulomatous lesions,
and connective-tissue tumors.
c) For frontal bone cysts, adequate exposure during
surgery is essential to allow complete removal of the mass and
capsule in order to prevent recurrences [4]. The eye-brow or
coronal approach with frontal craniotomy ensures satisfactory
exposure [5]. Long-term follow-up is needed given the risk of
local recurrence.
Epidermoid cyst of the frontal bone is rare. Preoperative
diagnosis is difficult, but CT and MRI images can suggest an
epidermoid cyst, thereby helping to plan the surgical approach.
Surgery is indispensable, and adequate exposure is required to
allow complete excision and avoid recurrence.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about juniper publishers: https://juniperpublishers.business.site/
Extradural Epidermal Inclusion Cyst Of Forehead: Case Report-Juniper Publishers >>>>> Download Now
ReplyDelete>>>>> Download Full
Extradural Epidermal Inclusion Cyst Of Forehead: Case Report-Juniper Publishers >>>>> Download LINK
>>>>> Download Now
Extradural Epidermal Inclusion Cyst Of Forehead: Case Report-Juniper Publishers >>>>> Download Full
>>>>> Download LINK HL