A Rare Case of Traumatic Leptomeningeal Cyst in Adult: Case Report-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Traumatic leptomeningeal cysts are a rare
complication of a childhood skull fracture. Clinical manifestations of a
childhood trauma are very rare in adults and usually presents as a
nontender subcutaneous mass with progressive neurological deficit and
seizures.
Keywords: Leptomeningeal cyst; Adult; Trauma; Seizures; Skull fracture
Abbrevations:
CT: Computed Tomography; MRI: Magnetic Resonance Imaging; CSF:
Cerebrospinal Fluid; T1WI: T1-Weighted Images; T2WI: T2-Weighted Images
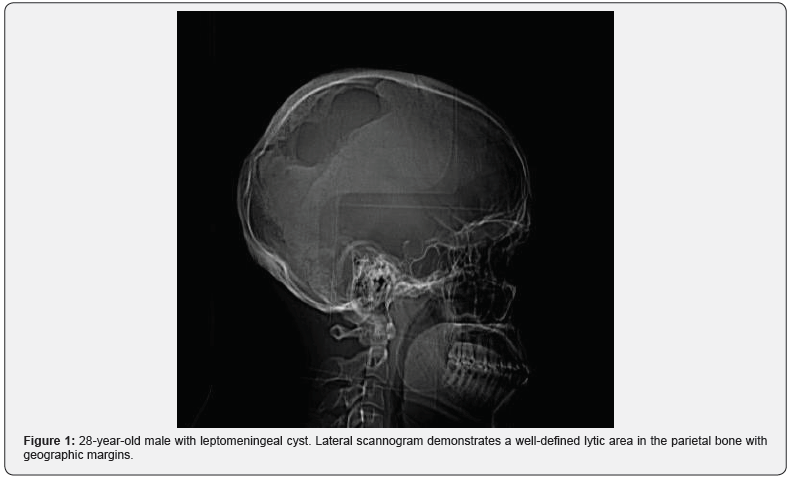
A 28-year-old male presenting with a gradually
increasing scalp swelling in the left parietal region over a long period
and seizures. The patient was conscious. On physical examination,
there was a cystic swelling over the left parietal prominence. The
swelling was compressible but non-tender and non-pulsatile. There was a
history of head injury during infancy (Figure 1-5).
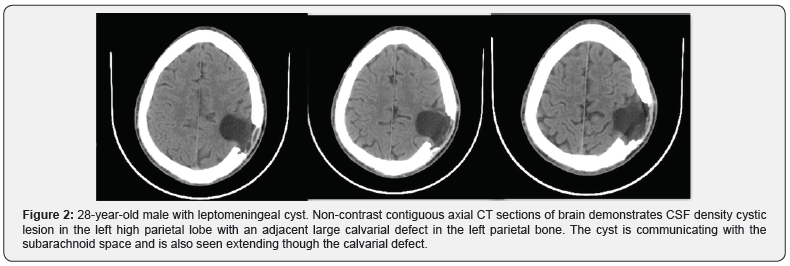
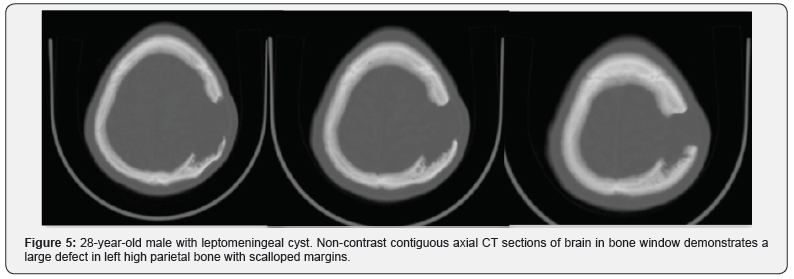
A non-contrast enhanced head computed tomography (CT)
examination was performed on a multidetector CT (Lightspeed
ultra, GE Medical Systems) and demonstrated a large calvarial
defect in the left parietal region with irregular and beveled margins.
An adjacent CSF density cystic lesion of size 42x41mm noted
in the left high parietal lobe. The cyst was seen communicating
with the subarachnoid space and also seen extending though the
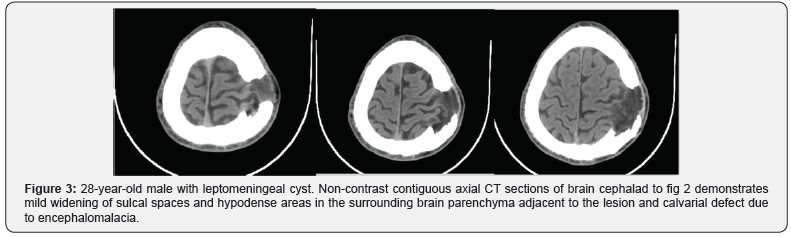
calvarial defect. Mild widening of sulcal spaces and hypodense
areas also noted in the surrounding brain parenchyma due to
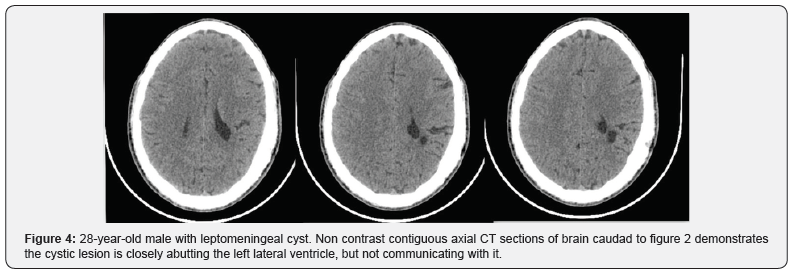
encephalomalacia. The cystic lesion was seen closely abutting the
left lateral ventricle with focal dilatation of the ventricle. But there
was no communication of the cyst with the ventricle. Corrective
surgery was done. The intraoperative and postoperative period
was uneventful.
Growing skull fractures usually occur due to severe head
trauma during the first three years of life, particularly in infancy.
Incidence reported is only.05 to.1% of skull fracture in childhood
[1,2]. Cause for growing skull fractures is multifactorial but the
main factor is tear in the dura mater. The pulsatile force of CSF
and pressure of growing brain will cause cerebral or subarachnoid
herniation through the dural tear which causes the fracture in
the thin skull to enlarge. This interposition of tissue prevents
osteoblasts from migrating, inhibiting fracture healing. The
resorption of the adjacent bone by the continuous pressure from
tissue herniation through the bone gap adds to the progression of
the fracture line (Tables 1-2). Table abbreviations: CT = Computed Tomography, MRI =
Magnetic Resonance Imaging, CSF = Cerebrospinal fluid, T1WI= T1-weighted
images,
T2WI= T2-weighted images. Table abbreviations: CT = Computed Tomography, MRI =
Magnetic Resonance Imaging, CSF = Cerebrospinal fluid, T1WI= T1-weighted
images,
T2WI= T2-weighted images.
The brain extrusion may be present shortly after diastatic
linear fracture in neonates and young infants [3] resulting in focal
dilatation of the lateral ventricle near the growing fracture. This
focal dilatation may be seen in adults which is also seen in this
case. This focal dilatation is reversible and may normalize after
surgical repair [4]. Cranial defects never increase if the underlying
dura is intact. Leptomeningeal cyst never occurs if the dura is
intact.
Another risk factor is severity of underlying trauma. A linear
fracture associated with hemorrhagic contusion of subjacent brain
suggests a trauma significant enough to cause dural laceration.
Cystic changes at the growing fracture site may be because of
cystic encephalomalacia. Post traumatic aneurysms and subdural
hematomas have also been reported to accompany growing skull
fractures [6,7]. Though most patients show damage to underlying
brain, this finding is not a prerequisite for the development of
growing skull fractures [8].
These skull fractures after reaching maximum extent will
cease to grow and remain stable throughout adulthood [2,5].
A depressed fracture usually does not become a growing
fracture [9] but a linear fracture extending from a depressed one
can become one [10].
A fracture with a diastasis of >4mm may be considered at
risk of developing a growing skull fracture [3,11,12]. But a post
traumatic diastasis of a cranial suture is an unusual site for a
growing fracture. Growing fractures can even be seen in usually
in linear fractures in thin areas of skull base associated with dural
laceration, for e.g.: Orbital roof, ethmoid plate, frontal sinus.
These fractures commonly present as a progressive, scalp
mass that appears sometime after head trauma sustained during
infancy. There may seizures and hemiparesis, but an asymptomatic
palpable mass may be the sole sign. The usual site is the parietal
region. A growing fracture at the skull base may present with
ocular proptosis or CSF rhinorrhea or otorrhea.
A plain radiograph may show a fracture line that crosses a
coronal or lambdoid suture, but it is usually limited to a parietal
bone [13]. CT or MRI demonstrates a cystic lesion near the fracture
site communicating with the subarachnoid spaces and extending
though the bony defect. Margins of bony defect may be beveled
or irregular. Adjacent brain parenchyma usually shows mild
encephalomalacia changes and focal atrophy. Gliosis may also see
in the adjacent brain parenchyma. On CT scan gliosis is seen as
hypodense areas. On MRI gliosis is seen as hypointense T1 and
hyperintense T2 signals.
Because of neurological deterioration and of seizure disorder
surgical correction of growing fractures is recommended.
Even though traumatic leptomeningeal cyst is rare in adults, it
should be considered in the differential diagnosis of intracranial
cystic lesions with adjacent calvarial defects.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about juniper publishers: https://juniperpublishers.business.site/

Comments
Post a Comment