Autologous Bone Marrow Derived Stem Cell (BM-MNC) Therapy for Pressure Injury in Spinal Cord Injury - A Pilot Study-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Ten Spinal cord injury (SCI) cases with grade 3 &
4 pressure injury (PI) were recruited. Five cases received autologous
bone marrow derived mononuclear cells (BM-MNCs) therapy and five
standard wound care. Significantly reduced surface area of PI in BM-MNC
treated group was observed at week 6 (p=0.04) and at week 9 (p=0.001) as
compared to standard wound care group. Similarly, significant reduction
of depth was observed in BM-MNC group at week 9 (p<0.05) and exudate
became significantly (p=0.001) lower from 3rd to 9th week. Clearance of
slough and formation of red granulation tissue was significantly higher
in BM-MNC group (p=0.001). The findings of this case series indicate
that the use of autologous BM-MNCs could be a feasible option for the
treatment of pressure injuries in SCI cases.
Keywords: Spinal cord injury; Pressure injury; Autologous bone marrow; Mononuclear cells
Abbrevations: PIs: Pressure Injuries; SCI: Spinal Cord Injury; MNCs: Mononuclear Cells; BM: Bone Marrow
Pressure injuries (PIs) are a common yet challenging
problem especially in people with Spinal cord injury (SCI) because of
immobility and anaesthetic skin. They are difficult to treat with
standard medical care and often recur [1-4]. Promising results have been
reported in the treatment of small series of mainly chronic
lower-extremity wounds with bone marrow-derived stem cells [5,6]. This
case series was aimed to obtain the preliminary data on the use of
autologous bone marrow derived mononuclear cells (BM-MNCs) to treat PIs
in terms of clinical outcome and procedure safety.
This study was conducted in the SCI unit, Department
of Orthopaedic Surgery in collaboration with the Department of
Transfusion Medicine, King George’s Medical University (KGMU), Lucknow,
India. We enrolled individuals with SCIs aged 16 to 60 years with stage 3
to 4PIs. Grading of PI was done as per taxonomy of NPUAP [7]. Exclusion
criteria were PIs with necrotic tissue that could not be removed on
baseline debridement, osteomyelitis, exposed blood vessels and nerves in
the wound,
and specific comorbid conditions likely to impair wound healing such as
diabetes mellitus, rheumatoid disease, and vasculitis.
About 3 hours before cell therapy, autologous bone
marrow (BM) (100ml) was obtained from the posterior iliac crest
aspiration. Mononuclear cells (MNCs) were separated from bone marrow
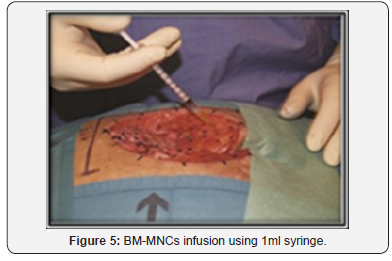
using plasma expresser. The BM-MNCs suspension was injected into the
wound bed by 1ml syringe. For injection, the wound was subdivided with a
grid into small areas of 1cm2. Infusion was performed into the wound
bed as well as sub
dermally at the borders of the wound. Wound dressings during
the entire study period were performed with moist gauzes twice
a day and followed up to 9 weeks (Figures 1-5).


Results
Physical wound healing outcomes were compared at weeks
3, 6, and 9. Significantly reduced surface area of PI in BM-MNC
group was observed at week 6 (p=0.04) which further reduced
at week 9 (p=0.001) as compared to standard wound care group.
Similarly, significant reduction of depth of PI was observed in
BM-MNC group at week 9 (p<0.05). The exudate was similar
(p>0.05) at the time of enrolment between both the groups
and became significantly (p=0.001) lower in BM-MNC group
from 3rd to 9th week. Clearance of slough and formation of red
granulation tissue was significantly higher in BM-MNC group
(p=0.001) (Table 1-3).
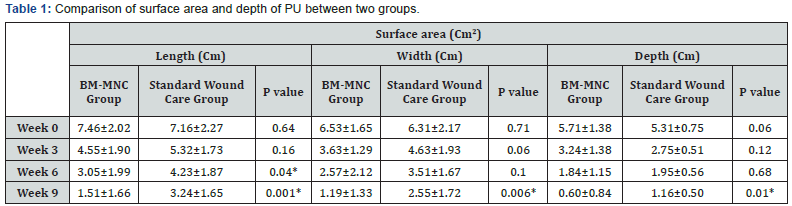
Values are presented as mean ± SD (Standard Deviation),
*: p<0.05 considered as statistically significant.
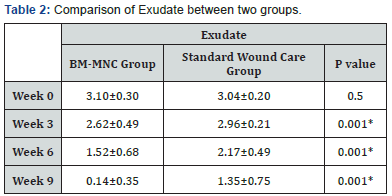
Values are represented as mean ± SD (Standard Deviation) 1Unpaired
t-test, *Significant (p<0.05).
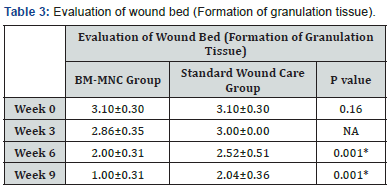
Values are represented as mean ± SD (Standard Deviation) 1Unpaired
t-test, *Significant (p<0.05).
Physical wound healing outcomes were compared at weeks
3, 6, and 9. Significantly reduced surface area of PI in BM-MNC
group was observed at week 6 (p=0.04) which further reduced
at week 9 (p=0.001) as compared to standard wound care group.
Similarly, significant reduction of depth of PI was observed in
BM-MNC group at week 9 (p<0.05). The exudate was similar
(p>0.05) at the time of enrolment between both the groups
and became significantly (p=0.001) lower in BM-MNC group
from 3rd to 9th week. Clearance of slough and formation of red
granulation tissue was significantly higher in BM-MNC group
(p=0.001) (Table 1-3).
PIs are a common yet challenging problem in patients with
SCI because they are difficult to treat with standard medical
therapy. Promising results have been reported in the treatment
of small series of mainly chronic lower-extremity wounds with
bone marrow-derived stem cells [5]. The rationale behind the
use of bone marrow derived cell therapy-is the fact that cells
in chronic wounds are phenotypically altered or senescent or
both. Therefore, they have a limited capacity to divide and are
less responsive to stimulation by growth factors [6]. MNCs from
a patient’s own bone marrow promote angiogenesis and this
seems to be a key factor for optimal healing of skin wounds.
Moreover, BM-MNCs secrete paracrine factors that could recruit
macrophages and endothelial cells to enhance wound healing.
The repair functions of BM-MNCs are thought to involve the
secretion of factors such as VEGF or FGF, which could help prevent
apoptosis, promote angiogenesis, assist in matrix reorganization
[8,9]. The use of autologous BM-MNCs was designed to avoid
problems of immunological rejection. The results observed in
terms of PI healing were independent of the number of cells
infused. The findings of this case series indicate that the use of
autologous BM-MNCs could be a feasible option for the treatment
of pressure injuries. The stem cell therapy proposed could avoid
major surgical intervention, especially if these wounds have not
responded to conservative and/or standard wound care.
The procedure of BM-MNC therapy was safe and well
tolerated by the subjects. The efficacy can be better commented
with larger sample size. But in this study, the results were highly
satisfactory.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about juniper publishers: https://juniperpublishers.business.site/
Comments
Post a Comment