A Rare Case of Frontal Lobe Abscess from Orbital Roof Blowout Fracture-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Orbital roof fractures are rare. These fractures are
usually associated with high velocity impact and polytrauma, and if
misdiagnosed, can have serious complications. This case demonstrates
that orbital roof fractures can be easily missed from plain film
radiographs and that clinical history and signs are of paramount
importance in assessing these cases. This case also emphasizes the
importance of multidisciplinary approach in trauma care.
Keywords: Frontal lobe abscess; Orbital roof fracture; Polytrauma
Orbital roof fractures are usually associated with
high impact trauma, accounting for approximately 1-9% of all
maxillofacial fractures [1]. These fractures are mostly associated with
other injuries in frontobasal trauma [2], although infants have a
relatively high incidence of orbital roof fractures because of absent
pneumatisation of the frontal sinus [3]. These fractures rarely present
in isolation and can be associated with significant complications
involving the eye, orbit, extraocular muscles, and brain.
Typically, the mechanism of injury for orbital roof
fractures is high-velocity/impact trauma such as motor vehicle/bike
accidents, and assaults. Facial lacerations as a result of the trauma
may be present along with periorbital oedema, ecchymosis, ocular
discomfort and epiphora. If there is involvement of the superior oblique
or rectus muscles, the patient may have limitation of vertical or
inward gaze or diplopia. Altered sensation in the distribution of the
supraorbital and supratrochlear nerves may be present, and if the
fracture is displaced, ex- or enophthalmos, hyper- or hypoglobus, or
proptosis may result. Timely diagnosis of orbital roof fractures is
imperative to prevent potential ophthalmological, neurological and
cosmetic morbidity. This is confirmed with radiology, preferably
computed tomography (CT).
A medically fit 34-year-old woman initially presented
to the Emergency department following a fall from her bike in which she
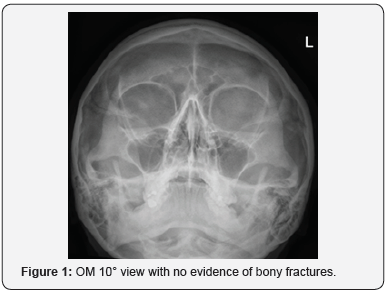
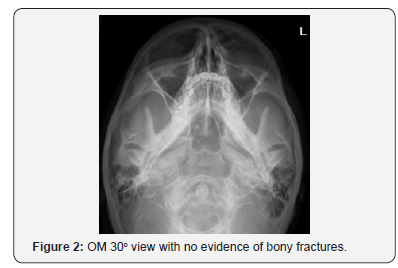
hit the left orbit with handlebar. Plain film radiographs (OM 10o and
30o) showed no evidence of any facial fractures (Figure 1 & 2).
Clinically, she had diplopia on lateral gaze associated with left eye
and a small laceration on the upper eyelid which was glued by A & E.
A 2-week review was planned by ophthalmology
She attended the eye casualty department 7 days after
the initial trauma complaining of restriction of movement.
Examination revealed restricted ocular motility and diplopia on
all direction of gaze left eye particularly downwards.
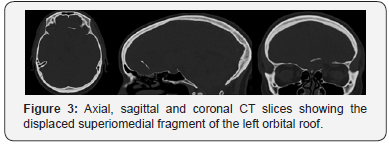
A CT scan revealed a blowout fracture through the
superomedial left orbital cavity with displaced fragments
projected 2cm into the left frontal lobe and she was referred
to Maxillofacial Surgery (Figure 3). Following discussion with
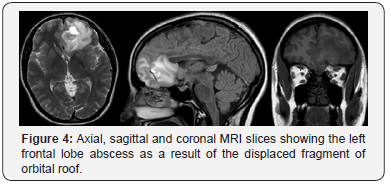
neurosurgery an MRI was arranged to exclude brain abscess.
This Figure 4 showed abscess formation around the left frontal
lobe. The patient had urgent bi-frontal craniotomy and drainage
of the abscess. Due to risk of infection of the bone or alloplastic
graft, no roof repair was performed. She remains well at 6
months follow up with no signs of pulsatile exophthalmos or
enophthalmos.
Discussion
Orbital roof fractures have been reported to account for
between 1% and 9% of facial bone fractures [1,4]. Isolated
orbital roof fractures are rare. The majority are associated with
other forms of neurologic injury. They are often the result of
high-energy impacts, such as motor vehicle accidents or falls
[5]. Non-displaced or minimally displaced orbital roof fractures
generally do not require surgical intervention and are managed
conservatively [3]. However, displaced orbital roof fractures
may be associated with significant neurologic, ophthalmologic,
and aesthetic morbidities, such as blindness, globe rupture,
eye immobility, altered sensation of the supraorbital and
supratrochlear nerves, CSF leakage, intracranial injury,
enophthalmos, exophthalmos, ectropion, entropion, infection,
diplopia, restricted extraocular movements, blepharoptosis,
orbital volume discrepancy, and those associated with the
presence of foreign bodies [1]. Surgical approaches to the
orbital roof present a risk of intracranial infection due to
the proximity of the frontal sinuses, concomitant dura tears,
and CSF leaks associated with pneumocephalus [6]. Surgical
approaches require multidisciplinary strategies involving
maxillofacial surgeons, neurosurgeons, and ophthalmologists.
Early reconstruction, within 10 days of trauma, by stabilizing the
midfacial fractures facilitates anatomical reconstruction because
bone margins remain intact and helps to reduce the need for
secondary operations and reduce the risk of infection [7].
Early recognition and treatment of orbital roof fractures can
reduce the incidence of intracranial and ocular complications. CT
scan plays a major role in the assessment of acute orbital trauma.
This case demonstrates how plain film radiographs alone have
a low sensitivity in diagnosing orbital roof fractures. Careful
clinical assessment and early consideration for CT scans are
important.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about juniper publishers: https://juniperpublishers.business.site/
Comments
Post a Comment