Periorbital Hemorrhage Secondary to tPA For Stroke Following Oculoplastic Surgery-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Introduction
Tissue plasminogen activator (tPA) is a proven
treatment for ischemic strokes when administered within 3-4.5 hours of
symptoms. Relative contraindications include minor or
spontaneously-improving stroke, seizure at onset, recent
gastrointestinal and urinary tract hemorrhage, pregnancy, recent major
surgery or serious trauma [1].
As these are relative contraindications, ultimately the provider makes
the decision to administer tPA based on analysis of risks and benefits.
This is a case of a periorbital hemorrhage in a patient receiving tPA
for ischemic stroke within 2 days of oculoplastic surgery. The case
highlights
a) The need to identify potential complications of tPA to the eye after oculoplastic surgery;
b) The benefit of understanding how to acutely manage periorbital/orbital hemorrhages provoked by tPA; and
c) The relative contraindication against tPA after
oculoplastic surgery when the caretaker is not trained in managing the
periorbital complications and when immediate subspecialty care cannot be
provided.
Case
A 76-year old male presented to a local emergency
room for left hemiparesis, right gaze deviation, and a NIHSS of 19. Less
than two days prior, he had undergone uncomplicated outpatient eyelid
surgery including bilateral blepharoplasty, lower eyelid ectropion
repair, and supraciliary brow lift. His past medical history included
hypertension and paroxysmal atrial fibrillation treated with 81mg daily
aspirin. His aspirin had been held for 1 week prior to his lid and brow
surgery.
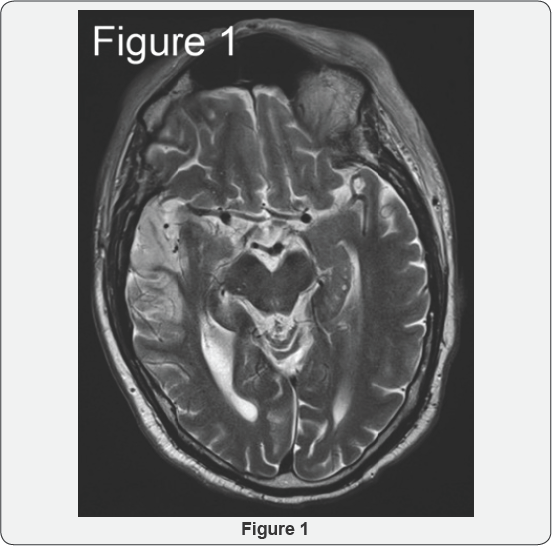
In the emergency department, CT imaging identified a
right middle cerebral artery ischemic stroke with a right M1 segment
occlusion, confirmed with MRI (Figure 1).
He received tPA and mechanical thrombectomy for the stroke, with rapid
alleviation of the hemiparesis. However, 3 hours after tPA
administration he developed progressively-worsening bilateral
periorbital ecchymosis with formation of a tense hematoma on the left.
Assessment by an on-call ophthalmologist found that the left eye had no
light perception, raising concern for acute hemorrhage within the orbit
compressing the optic nerve. The sutures were removed from the left
blepharoplasty and ectropion incisions, which allowed egress of an
eyelid and orbital hematoma (Figure 2A-2C).
By that evening, the patient was noted to have 20/200 vision with
normal intraocular pressure on the left side. He received appropriate
post-stroke care and was discharged 4 days later.
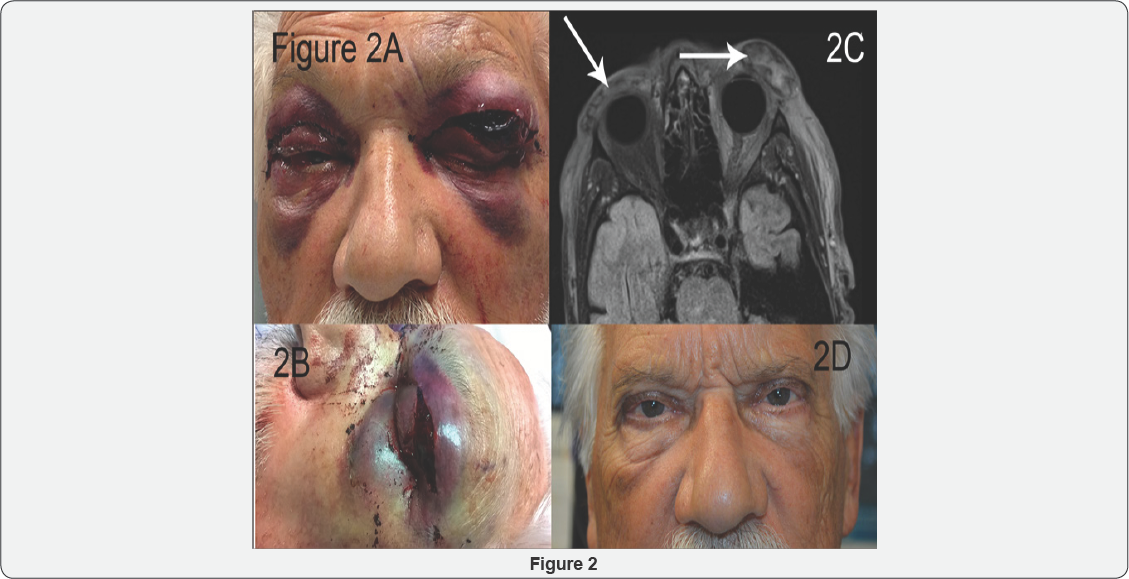
One week after the initial surgery, the remaining
hematoma was surgically evacuated from the left eyelid and the surgical
incisions were resutured. At follow up 3 months later, his vision had
returned to baseline, with adequate eyelid healing and no significant
sequelae (Figure 2D).
Few reports identify intraorbital and periorbital
hemorrhages after tPA. Thrombolytics after myocardial infarctions have
caused orbital hemorrhages [2-4]. Intractable bleeding from a blepharoplasty wound has occurred after thrombolysis for a pulmonary embolism [5]. Sheth & Lee [6] described orbital hemorrhage in a patient who received tPA for stroke after recent orbital trauma [6].
The Americal Society of Aesthetic Plastic Surgery estimates over
165,000 eyelid surgeries are performed yearly in the United States [7].
The periorbital region significantly increases the risk of bleeding.
Therefore, despite the rarity of a periorbital hemorrhage due to tPA for
stroke after oculoplastic surgery, trainees and physicians caring for
such patients need to consider the anatomy and vision-threatening
consequences of hemorrhage around the eye, and the appropriate
management if they encounter this complication.
In a large survey of ophthalmic plastic surgeons, the
risk of postoperative hemorrhage after upper or lower lid
blepharoplasty was estimated to be 0.055%, most within the first 24
hours [8].
Hemorrhage that accumulates posterior to the orbital septum can cause
orbital compartment syndrome. Orbital compartment syndrome is a
potentially blinding condition of increased intraobital pressure,
leading to stretching of the optic nerve, compression of the vessels
supplying the optic nerve, elevated intraocular pressure, reduced venous
outflow from the eye, and orbital ischemia. Symptoms include vision
loss, pain, nausea, and vomiting. Signs include proptosis, extensive
periorbital edema with ecchymosis, tense eyelids, loss of color vision,
ophthalmoplegia, and an afferent pupillary defect [8].
In our case, the large periocular hematoma made
bedside exam challenging, even for a trained ophthalmologist. Concerning
features included the progressive proptosis, tense eyelids, declining
visual acuity, and afferent pupillary defect. Prompt release of the
sutures from his incisions allowed external decompression rather than
intraorbital progression. This demonstrates the importance of emergent
treatment of any significant hemorrhage around the eye after tPA.
While imaging helps diagnose the area of periocular
hemorrhage, it is not appropriate to delay prompt treatment of orbital
compartment syndrome while awaiting imaging. If an ophthalmologist is
not emergently available, treatment should be undertaken by the covering
neurologist or emergency department physician. Permanent vision loss
can occur within 60-90 minutes after an orbital hemorrhage [9]. Prompt treatment may preserve vision [6].
In the case of tense orbital hematoma formation in the perioperative
period, simple removal of the sutures to allow the hemorrhage to drain
is crucial. A lateral canthotomy and cantholysis to further decompress
the orbit is likely beyond the scope of the neurologist, but these
procedures are known to emergency room physicians. Bleeding from the
opened incisions is likely to occur, but can then be managed by
subspecialty services when they arrive, with topical pro- thrombotics or
cautery [5].
This case highlights that thrombolysis with tPA can
disrupt the newly formed clots of the upper eyelid and brow within the
first 1 week after upper eyelid blepharoplasty and brow ptosis repair.
Although these oculoplastic procedures are designated as minor rather
than major surgery, tPA-related orbital hemorrhage after such surgery
may cause permanent vision loss from compartment syndrome.
The risk of persistent debility or death due to
stroke certainly outweighs the risk of orbital or periorbital
hemorrhages for cases in which treatment for potential hemorrhage is
readily available. However, in settings in which timely treatment of a
periorbital or orbital complication cannot be provided, physicians
providing tPA should view recent oculoplastic surgery as a relative
contraindication. We recommend physicians consider the risk of tPA after
oculoplastic surgery, develop the skill set of suture removal to allow
basic decompression, and consult ophthalmology early in the tPA
administration so that they can provide emergent care if needed.
a) Administration of tPA for ischemic stroke can
provoke vision-threatening periocular bleeding after even minor
oculoplastic surgery.
b) The tPA provider should be vigilant for hematoma
formation in patients after periocular surgery, and be prepared to
release the eyelid sutures and notify subspecialty services promptly to
decompress the wounds.
c) Recent oculoplastics surgery should be considered a
relative contraindication for tPA if the provider is unfamiliar with
acute periocular hemorrhage management or if subspecialty services for
the eye or orbit are unavailable.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment