Percutaneous Vertebroplasty as a Treatment for Osteoporotic Vertebral Compression Fractures-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Percutaneous vertebroplasty is a minimally invasive
procedure for the treatment of osteoporotic and neoplastic vertebral
compression fractures; this procedure involves the injection of bone
cement directly into the fractured vertebral body. The purpose of this
study was to evaluate the efficacy of percutaneous vertebroplasty for
patients with painful osteoporotic vertebral compression fractures. This
was a retrospective single-center study; the total number 74
percutaneous vertebroplasty was performed in 41 patients with
osteoporotic vertebral body compression fractures of the I and II
degrees. Of these 41patients, 5 were male (12%) and 36(88%) were female;
the average age of the patients was 66 years (range, 55-78 years). The
overall procedure time was 51.2 ± 4.2 (range, 34-55)min. The average
cement volume injected into vertebra was 4.5 ± 0.54 (range, 3.4-6.0)ml.
The mean follow-up was 16.0 ± 4.2 (range, 12-24) months. All patients
achieved substantial pain relief after surgery; the Visual Analogue
Scale (VAS) score decreased significantly from a pre-operative value of
8.4 ± 1.2 to a post-operative value of 2.0 ± 0.2 and was maintained at
2.2 ± 0.4 at the final follow-up (p < 0.01). Our study confirmed that
percutaneous vertebroplasty is effective treatment modality for
osteoporotic vertebral compression fractures, which offers short and
long-term statistically significant benefits in decreasing pain and
increasing mobility.
Keywords: Osteoporotic vertebral compression fractures; Percutaneous vertebroplasty
Osteoporotic vertebral compression fractures (OVCFs)
are the most common single osteoporotic fractures worldwide,
constituting an integral part of the osteoporotic syndrome; they occur
in 30-50% of people over the age of 50 [1].
The OVCFs have a negative impact on health related quality of life and
are associated with increased mortality. Conservative management,
including bed rest, pain relievers, bracing and physical therapy, may
fail to relieve pain and frequently lead to prolonged immobilization,
depression and a substantial negative impact on life quality.
Percutaneous vertebroplasty (PVP) is a minimally invasive procedure for
the treatment of OVCFs; it consists of percutaneous injection of
biomaterial, such as Polymethyl methacrylate (PMMA), into the fractured
vertebral body [2].
The procedure is well tolerated even under local anesthesia.
Biomechanical testing has shown that PVP can restore strength and
stiffness of the vertebral body to the pre-fracture levels. The
advantages of PVP included are following: reduction in pain, disability,
and analgesic use; as well as stabilization of the vertebral fracture [3].
The short-term risk factors of PVP are associated with a cement leakage
into the spinal canal or into the venous system; the long-term risk
factor of PVP is incidence of new vertebral fracture. The PVP as a
treatment mode for painful vertebral compression fractures provided
long-term therapeutic effects in 70-95% of the patients [4]. Cost-effective analysis revealed that PVP is most cost-effective treatment procedure in patients with OVCFs in Japan [5].
Thus, the aim of our study was to evaluate the immediate
post-interventional and long-term outcomes after PVP in terms of pain
relief.
Data were collected retrospectively from the records
of patients treated between 2015 and 2017 at the department of
“Traumatology, orthopedics, neurosurgery with military surgery“ of the
Tashkent Medical Academy (TMA). The study was executed in compliance
with the Helsinki Declaration and local data protection regulations of
TMA. The database included data from patients who signed an informed
consent form allowing the use of their clinical data for research
purposes. Indications for PVP were the presence of single or multiple
vertebral compression fractures of vertebral bodies of the I and II
degree with a strong pain syndrome, along with osteoporosis, which was
preoperatively diagnosed by dual-energy X-ray absorptiometry (DXA).
Patients undergoing vertebroplasty for other conditions such as
vertebral metastasis, multiple myeloma or traumatic fractures of the
spine were excluded. Contraindications of PVP
were following: osteomyelitis, discitisor active systemic infection;
unstable spinal fracture, patients with diffuse idiopathic skeletal
hyperostosis and ankylosing spondylitis; severe uncorrectable
coagulopathy; impaired cardiopulmonary function; neurologic deficits and
spinal cord compression syndrome; bone fragment retropulsion; allergy
to bone cement or opacification agents. The following examinations were
made in all the patients prior PVP: detailed clinical evaluation,
including a the neurological status; blood test with extended
coagulogram; imagining modalities such as such X-ray, magnetic resonance
tomography (MRT) or multislice computed tomography (MSCT). Osteoporosis
was preoperatively diagnosed by dual X-ray absorptiometry in all
patients. In order to evaluate the severity of the pain, the visual
analog scale (VAS) was used; this system grades pain based on the
following: 0=absence of pain, 2 = mild pain, 4=moderate pain, 6=severe
pain, 8=extreme pain 10=worst pain. The cemented proportion of the
vertebral body was determined using volumetric analysis of the
postoperative CT scan of the treated levels.
Statistical analysis was performed using SPSS for
Windows version 18.0 (SPSS Inc., Chicago, IL, USA). All variables were
analysed using descriptive statistical methods. Data are presented as
the mean and standard deviation for continuous variables and as
percentages for categorical variables. Comparisons of pain outcomes pre-
and postoperatively were made using a paired t test. Differences were
considered statistically significant when p < 0.05.
The preoperative prophylactic antibiotic cefazolin
1g, was administered intravenously. The procedure was performed under
local anesthesia. The transpedicular approach was used to access the
collapsed vertebral body in the thoracic and lumbar spine. The vertebral
venography has been used for the identification of potential routes of
cement venous leakage. The cement is composed of methyl methacrylate and
monomer liquid, which were mixed together. Cement injection was done
under continuous lateral fluoroscopic control; it was injected using a
13-gauge cannula. The fractured vertebral body was gradually filled with
cement until admissible endpoints. Cement injection was interrupted in
case of venous leakage into the veins or spinal canal. Patients were in
supine position within 1.5hour after the procedure, the assessment of
vital functions and neurological status were examined in every 15
minutes. The control MSCT or CT of the treated level was performed in
the first 2-3 days after the procedure.
A total of 41 patients (36 females and 5 males) met
the inclusion criteria and were treated with PVP and then included in
the follow-up program that is still going on. The total number 74
percutaneous vertebroplasty was performed in 41 patients with traumatic
compression fractures of vertebral bodies of the I and II degree. Of
these 41, 5 participants were male (12%) and 36(88 %) were female; the
average age of the patients was 66 years (range, 55-78 years). The
average operative time was 51.2 ±4.2 (range, 34-55)min. The average
cement volume was 4.5 ± 0.54 (range, 3.4-6.0)ml. The mean follow-up was
16.0 ± 4.2 (range, 12-24) months. The evaluation of the results of
treatment was carried out according to the following criteria: dynamics
and severity of pain syndrome prior and after percutaneous
vertebroplasty, motor activity of the patient, and dependence on
analgesics. All patients achieved substantial pain relief after surgery.
The VAS score decreased significantly from a preoperative value of 8.4 ±
1.2 to a post-operative value of 2.0 ± 0.2 and was maintained at 2.2 ±
0.4 at the final follow-up (p < 0.01). The extravasation of cement
into the venous plexuses was noted in 1 patient, which was the reason of
occlusion of small branches of the pulmonary arteries, and clinical
presentations of this case was asymptomatic. No other complications were
encountered. All patients were able to sustain rapid mobilization
within 12- 24h after procedure, and the mean hospitalization length
after PVP was 3.5 days (range 3-5). The long- term results revealed that
all patients had significantly improved mobility, and by the end of the
first postoperative month and mainstay during following 24 month, there
were not any subsequent vertebral fractures. In additionally, during
the follow up period the majority of patients reported that decreased
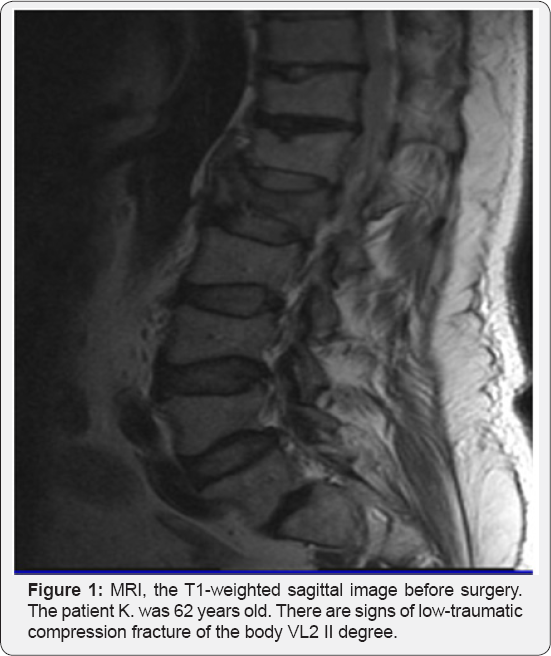
usage pain relief medicines or not used (Figure 1 & 2).

Discussion
To date, there are several vertebral augmentation
modalities are applied to reduce pain and stabilize compression
fractures of the spine; over the decade, the PVP and balloon kyphoplasty
(BKP) are used and the novel procedures are radiofrequency kyphoplasty
and percutaneous implant techniques [6].
The advantage of PVP/PKP in comparison to conservative management or
open surgery has been well established in terms of decreasing pain and
improving QOL of patients with OVCFs [7].
Nevertheless, the complications of PVP / PKP are associated with the
risk of cement leakage during procedures. The spinal extravasation can
lead to cord and nerve injury as well as paravertebral soft tissue and
intervertebral disc damage; the venous extravasation into the epidural
and vertebral veins can cause cardiac and pulmonary cement embolization.
In our series, the incidence of embolism of the pulmonary arteries was
2.34% (1/41), which was significantly lower then recently reported in
literature for PVP/PKP, which was ranged between 3.5% and 23% [8].
Therefore, the early postoperative clinical and radiological (CT or
MSCT) examinations are recommended to check the proper implants
position, but also to detect the possible cement migration.
The controversy exists as to whether PVP/PKP can
increase the risk for new OVCFs during follow-up .The experimental
biomechanical studies demonstrated that PVP/PKP increased stiffness and
strength. Besides, the augmented vertebrae after PVP/PKP increased
loading in adjacent vertebrae, inducing subsequent fractures. To resolve
the issues, to date the some modifications of injected cements are
being developed in experimental studies. Schroder et al. [9],
conducted experimental study to examine the influence of adding 10 and
30vol% isotonic saline on the biomechanical properties of PMMA
vertebroplasty cement. The result of this study demonstrated that
compressive stiffness of PMMA-based vertebroplasty cement could be
reduced to almost a third by the addition of saline. The probable
explanation is an increase in microporosity of cement, which can reduce
the risk of subsequent vertebral fractures [9]. Another investigation by Liu et al. [10]
tested newly designed CPB cement for replacing the PMMA in PVP and PKP.
The biomechanical, biocompatibility, osseointegrative and handling
properties of CPB were systematically evaluated in vitro and in vivo.
The results of this investigation demonstrated that the biological
performance of CPB outperformed the non-degradable PMMA. The authors
concluded that CPB has revolutionary potential to replace the PMMA in
the applications such as PVP and PKP [10]. Certainly, the above-mentioned two experimental studies are required further evaluation in clinical settings.
Our study demonstrated that PVP offers statistically
significant short and long- term benefits in decreasing pain and
increasing mobility for patients with OVCFs. The perioperative
complication of cement leakage observed only in one patient, there were
not any subsequent vertebral fractures in long- term follow-up.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment