Delayed Progressive Cauda Equina Syndrome after Transverse Sacral Fracture: A Case Report-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Transverse sacral fractures are infrequent injuries
that often cause neurological impairment referred to as cauda equine
syndrome. To the best of our knowledge, the onset of neurological
symptoms can be delayed up to 2 months. We report a case of isolated
transverse sacral fracture through S2-S3 which caused minor symptoms
after 6 days. Major neurological disability appeared with a 3 months
delay. A limited laminectomy was performed with good clinical results.
The 3 months delay appeared to be the longest compared to available
literature.
Keywords:Transverse sacral fracture; Laminectomy; Caudaequina syndrome; Delay
Transverse sacral fractures are rare. They occur
after low or high energy trauma, with clinical manifestations that
include neurological dysfunctions. According to the literature, these
symptoms can be delayed [1-4]. To our knowledge, the literature reports
only 2 cases with neurological signs that became significant as late as 2
months after trauma [1]. There is no clear consensus on how to manage
these fractures [4-6]. We report a case of isolated transverse sacral
fracture through S2-S3 which caused significant neurological symptoms 3
months after trauma. We compare our observation to the available
literature.
A 50-year-old woman presented to our emergency
department with pain in lumbo-sacral region two days after falling in
the stairs (approximately 3 meters) with impact on her lower back. She
had no relevant medical history. The pain increased in seated and supine
position. Bowel, bladder, sphincters and lower limbs were clear of any
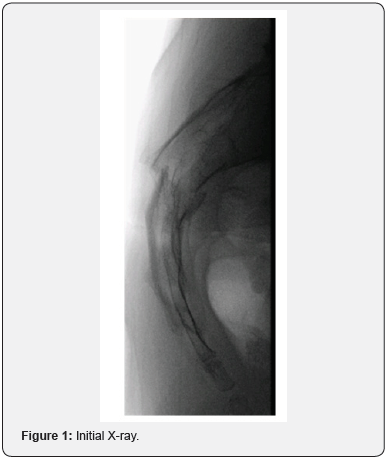
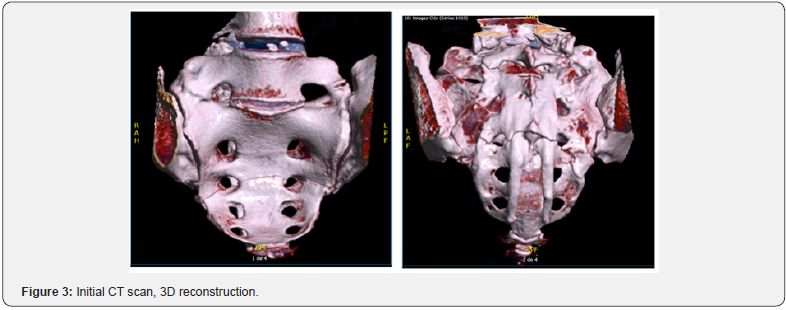
symptom. Perineal sensation was normal. X-rays and CT scan images
revealed a transverse sacral fracture through S2-S3 junction with no
vertical extension. The distal fragment was flexed and anteriorly
displaced of 5mm. The canal was enchroached by fragments from the
anterior and posterior aspect of the sacral canal (Figure 1-3). She was
discharged with painkillers and followed in outpatient clinic.

At day 6 after trauma, she had an additional symptom of
saddle hypo-esthesia. Bladder, sphincters and lower limbs were
still normal. The conservative management was continued
and surgical treatment was to be considered only in case of
neurological deterioration. At 6 weeks, pain had decreased but
saddle numbness persisted with no aggravation nor additional
symptom.
Urinary incontinence appeared at 3 months post trauma and
was complete within 2 weeks. CT scan imaging was repeated and
showed advanced consolidation with a callus that was slightly
larger than on previous workups. This suggested increased
canal compression (Figure 4). The patient underwent S2-S3
laminectomy. Urinary dysfunction was almost back to normal
on the day after surgery. All neurological symptoms recovered
within two weeks following surgery.

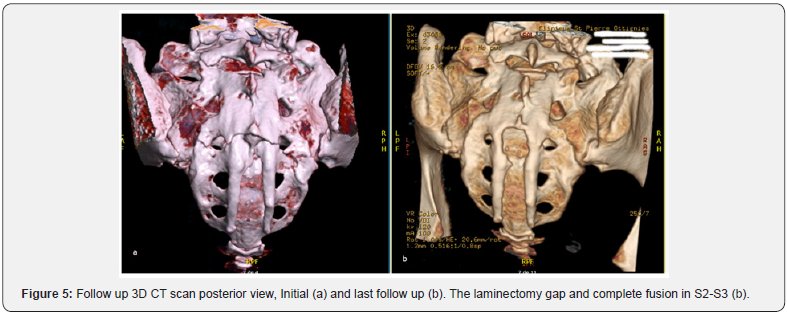
At last follow up (12 months after initial trauma), the
patient’s neurological status was normal. She had resumed
regular jogging and swimming with no discomfort. Final CT scan
showed full fusion of the fracture and post laminectomy status in
S2-S3 (Figure 5).
Discussion
Several classifications have been proposed for sacral
fractures but none of them encompasses all the fractures’
patterns encountered in clinical practice. Roy-Camille et al. [7]
described suicidal jumper’s fractures that occurred at S1-S2 level
comprising transverse and vertical orientations (H, U patterns).
Their study classified 3 types of fractures.
a) Type 1: Anterior flexion fracture.
b) Type 2: Anterior flexion fracture with posterior
displacement of proximal fragment.
c) Type 3: Extension fracture with anterior displacement
of proximal fragment.
Denis et al. [8] classified sacral fractures in 3 vertical zones:
zone 1 lateral to the foramina, zone 2 involving the foramina
and zone 3 the sacral canal [4,5,8]. Zone 3 lesions can be subclassified
into vertical or transverse fractures [5].
Shmidek et al. [9] divided transverse sacral fractures
according to the level: high (through S1-S2) versus low (through
S3-S5) [5,9]. High fractures are caused by indirect high energy
forces (motor vehicle accident, suicidal jump) and are usually
unstable due to a three-dimensional configuration (H,U or Ttypes),
whereas low fractures result from direct trauma (fall
onto buttocks) and are likely to be stable [2,5]. Given the sacroiliac
weight transmission, these fractures are stable if sacrum
and sacroiliac joint above S1 foramen are intact [5].
Our patient fell onto her buttocks and presented an isolated
transverse fracture through S2-S3 that can be classified as a
low transverse Zone 1-2-3 fracture. It has been observed that
neurologic injury is most frequent in fractures involving Denis
Zone 3 (60%) [4,5,10]. Denis et al. [8] found the risk to be greater
in transverse fractures than in vertical ones [2,8]. Usual clinical
repercussions are bowel and bladder dysfunction, sphincters
incontinence, L5/S1 deficits and saddle anaesthesia resulting in
cauda equina syndrome [2,4,5]. According to the literature, these
neurological signs are often variable and delayed [1,3], while
local pain is always noted from the beginning [11]. The delays
for neurological symptoms range from a few days to 2 months as
reported by Lee et al. [1], with most neurologic deficits appearing
at the same time. Aresti et al. [4] report a case with progressive
symptoms starting with isolated S1 radicular symptoms at day
10 after trauma followed by urinary dysfunction and saddle
anaesthesia 6 weeks later. In the present case, saddle hypoesthesia
appeared at day 6 and remained stable until urinary
incontinence appeared at 3 months post trauma.
After physical examination, transverse sacral fractures can
be confirmed and evaluated on plain X-rays. However, CT scan
imaging is the best way to avoid misdiagnosis and allow for
thorough description and classification [2,11].
The literature does not provide precise treatment guidelines.
In the case of transverse sacral fracture with neurological
impairment, there is controversy between surgical and
conservative management. Both approaches do result in recovery
rates as high as 80% [6]. Surgery has been advocated in case of
high energy trauma, neurologic deficit, displacement exceeding
1cm, canal encroachment and fracture instability [2,5,6].
Timing of surgery is still debated and there’s no clear evidence
whether early or late intervention is best [2,4]. As to the surgical
technique, decompression alone by wide laminectomy has been
proposed in case of neurological impairment with canal stenosis
[1,2,4-6]. Internal fixation is recommended in case of instability
or major displacement [2,4,6].
In the present case, the early neurologic impairment was
considered as moderate and priority was given to conservative
treatment. Surgery was indicated by the appearance of
incontinence. Laminectomy was performed considering the canal
encroachment while stabilization was unnecessary: fusion was
already obtained, especially in the anterior column. Anatomical
and clinical results were satisfying at final follow up.
Isolated transverse sacral fracture is rare and likely to occur
after low energy direct trauma. Clinical manifestations include
local pain and cauda equine signs that are variable in time
and severity. Mild neurological deficits can deteriorate even 3
months later. Management should be adapted to each patient,
according to the fracture pattern and neurological impairment.
Sacral decompression can still result in good improvement, even
at a delayed state.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about juniper publishers: https://juniperpublishers.business.site/
Comments
Post a Comment