Conscious Sedation in Plastic Surgery: Patient Safety and Cost Reduction Midazolam/Meperidine Conscious Sedation-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Background: Conscious sedation is an
anesthetic modality used in different procedures, among which are
plastic surgeries. This study evaluated the efficacy and safety of the
IV Midazolam - IM Meperidine conscious sedation protocol.
Methods: Adult patients undergoing elective
cosmetic surgeries were enrolled. Patients were excluded if they had a
history of cardiac or respiratory disease or in case of pregnancy.
Patient anxiety, nausea, and pain were evaluated during and after
surgery. Physician satisfaction and reported intraoperative level of
sedation were also assessed. Operative time, midazolam dose, and the
lowest hemoglobin saturation level in oxygen were noted. The primary
outcome was postoperative recovery time while cost reduction and post
operative complications were considered as secondary outcome measures.
Results: 173 patients were recruited. 61.8%
under went rhinoplasty procedures and 13.8% under went blepharoplasty.
Mean recovery time was 196 minutes. Age was the most significant
predictor of recovery time. Older patients recovered faster (p=0.019),
were less anxious preoperatively (p=0.003) and had less postoperative
pain (p=0.007) and nausea (p<0.0001). Higher dose of Midazolam were
associated with more intraoperative anxiety (p=0.02) and an increased
postoperative nausea (p=0.047) and emesis (p=0.032). We also can note
that High (7-14 glasses/week) alcohol intake was associated with slower
discharge (p=0.022).
Conclusions: The IM Meperidine-IV Midazolam
conscious sedation protocol in plastic surgery operations in the
one-day-surgery setting seems to be safe reproductible and cost
effective.
Conscious sedation or "Procedural Sedation and
Analgesia (PSAA)” is the modality in which sedative agents are
administered (with or without analgesics) to induce a minimally
depressed level of consciousness sufficient to perform certain
procedures. The strict definition requires that the patient be
responsive to verbal command at all times and maintain airway patency
and protective reflexes. It has been used across numerous specialties to
perform invasive surgical, endoscopic, and intravascular procedures of
limited durations; these include orthopedic, oral, plastic,
neuroendovascular, cardiac, gastric, and radiological procedures [1-8].
The technique has been widely employed in plastic surgery thanks to the
advantages it has over other anesthetic modalities, namely lower costs,
faster recovery, better patient and surgeon satisfaction, and lower
morbidity [9].
The surgical use of conscious sedation requires the concomitant
administration of local anesthetic agents in order to achieve
appropriate analgesia in the intraoperativeas well as the postoperative
setting. Conscious sedation technique aims at attaining three main
objectives when employed in plastic surgery: to reduce or eliminate the
pain associated with injection of local anesthetic, to reduce or
eliminate patient apprehension, and to reduce or eliminate recall of the
operation [10].
This study aims to describe and evaluate the safety and efficacy of an
IV Midazolam-IM Meperidine (Pethidine) conscious sedation protocol that
has been in use for three decades over thousands of patients at our
institution in patients under going elective cosmetic surgeries.
Patients and Methods
Ethics statement
Institutional Review Board approval was obtained.
Patients aged eighteen years or older undergoing elective surgical
procedures under conscious sedation provided their written informed
consent to participate in the study.
Study design and patient selection
This prospective study recruited patients at the
Department of Plastic Surgery in major tertiary University Hospital in
Beirut from November 2013 to December 2014. Patients aged eighteen years
or older undergoing elective cosmetic surgical procedures, in which the
Midazolam/Meperidine conscious sedation protocol is usually used, were
approached and the study objectives were explained to each patient..
Patients were excluded if they had a history of cardiac or respiratory
disease or in case of pregnancy.
Surgical techniques and conscious sedation protocol
Premedication was administered at the day care unit
around thirty minutes before surgery as an intramuscular injection of
Meperidine 75mg, Haloperidol 2.5mg, and Atropine 0.25mg. Surgical
procedures were conducted in a specially conceived operating room where
the primary surgeon and his assistant
- a resident - operate in the presence of one circulating nurse.
Anesthesiologists were located nearby, readily available for
intervention upon request.
In blepharoplasty procedures, oxybuprocaine eye drops
(Cebesine 0.4%) were used in the immediate preoperative period while in
rhinoplasty procedures, a lidocaine-based gel was applied intranasally
before in filtration by the local anesthetic solution (Lidocaine 1% with
1/200,000 epinephrine).
After positioning and proper draping, a direct
intravenous Midazolam dose (1 to 3 mg) was administered seconds before
the infiltration by the local anesthetic solution. Sedation level could
be readily verified through mild non-verbal stimulation by gently
touching the patient's eyelashes and looking for a reflex response.
Infiltration was then undergone, and in rhinoplasty, the nose was packed
with gauze soaked in Lidocaine-based gel. Oxygen saturation level was
monitored throughout the procedure and the levels of sedation and
anxiety were constantly evaluated. If the patient became or remained
conscious and/or anxious, the surgeon called for additional midazolam as
needed. On the other hand, if the patient's respiratory rate and/or
oxygen saturation decreased, the patient was verbally instructed to
breathe deeply. In case the patient was not responsive to verbal
stimulation, a brief jaw-thrust maneuver was applied, or, very rarely, a
Guedel cannula could be inserted for airway patency or reverse
medication could be administered.
The postoperative period consisted of a minimum of
three hours of rest during which the patient wasn't allowed nothing per
orem. After this recovery period, when the patient could autonomously
walk and eat, he/she were considered ready for discharge.
Patient and surgeon questionnaires
Patient anxiety was evaluated before and after
premedication (auto-evaluation and evaluation by the physician).
Physician satisfaction was noted on a scale from zero to ten, as well as
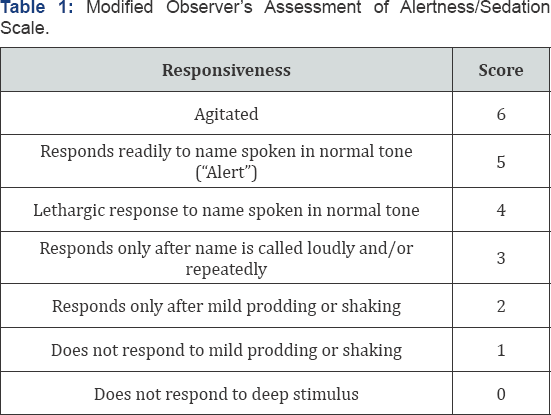
intraoperativelevel of sedation (Modified Observer's Assessment of
Alertness/Sedation Scale) [11]
at four different timepoints during surgery: 1- at infiltration of the
local anesthetic, 2- fifteen minutes after the infiltration, 3- during
lateral osteotomy (only in rhinoplasty procedures), and 4- during cast
placement (only in rhinoplasty) (Table 1).
Intraoperative nausea or emesis was also assessed. Operative time,
midazolam dose, and the lowest hemoglobin saturation level in oxygen
were noted. Postoperative anxiety, nausea/emesis, and pain were
evaluated using a questionnaire employed in a study by Hasen et al. [12].
The designated primary outcome was recovery time which corresponded to
the time needed to regain orthostatic autonomy after the end of the
operation. Discharge time - time from the end of the operation until
discharge - depended less on the autonomy of the patient than on
administrative and logistic issues, which meant that it was less related
to the recovery from sedation than recovery time. Cost reduction,
unintended admissions, pain, anxiety, nausea, emesis, and patient recall
were considered the secondary outcome measures.
Statistical analysis
Statistical analyses were done using Stata.
Kolmogorov- Smirnov test was undergone to test for the normality of the
distribution of independent variables. Statistical relationships were
studied between dependent variables and independent variables.
A total of 173 patients were recruited of which 144
were females (83.2%). Mean age was 35.2 years (95% confidence interval
[32.8; 37.6] years) (Table 2).
107 patients (61.8%) underwent rhinoplasty procedures, 24 patients
(13.8%) underwent blepharoplasty procedures and 42 patients (24.3%)
under went other procedures (liposuction/fat grafting, otoplasty, and
other procedures). Mean operative time was 59.5 minutes (95% confidence
interval (CI) 56.3-62.8 minutes). Mean recovery time was 196 minutes
(95% CI 181-212). None of the patients required intraoperative
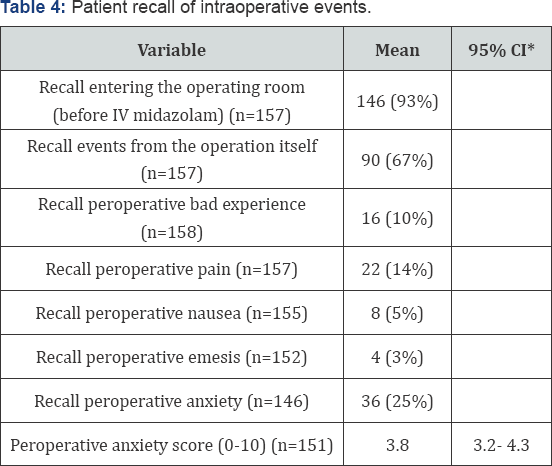
anesthesiologist intervention or an unintended admission. 90% of
patients recalled some events from the operation while only 10% recalled
an intraoperative bad experience. 10.5% of patients reported
postoperative nausea. However, when asked to rate their nausea from 0 to
10, only 15.4% of 155 patients reported a score of more than 5.
Postoperative emesis was reported in 14% of patients. One patient
presented to the emergency department 4 hours after discharge for
extrapyramidal symptoms (trismus). She was successfully treated with a
50mg intramuscular dose of promethazine (Phenergan®). Other results are
summarized in Tables 2-4.
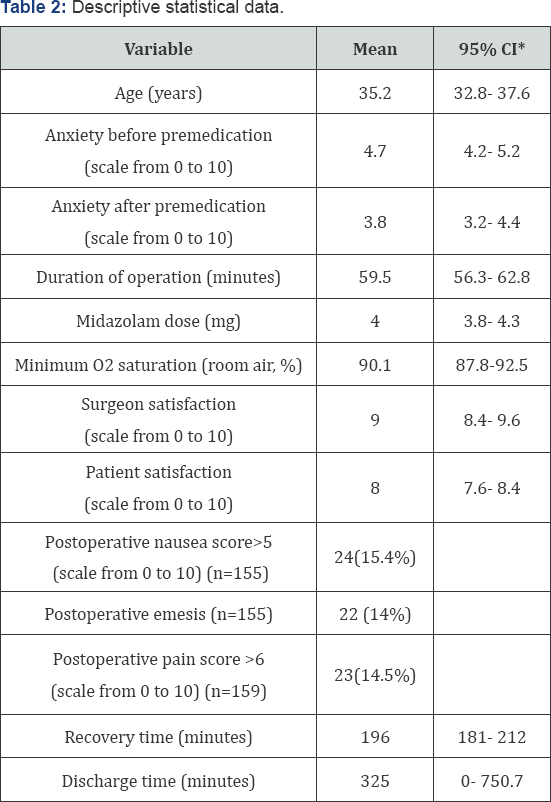
*CI: Confidence Interval.

*CI: Confidence Interval.
*CI: Confidence Interval.
Primary and secondary outcomes
In univariate analyses, age was the most significant
predictor of recovery time. Older patients recovered faster (p=0.019),
and were discharged faster (p=0.009). They were less anxious
preoperatively (before (p=0.003) and after premedication (p=0.092), had
less postoperative pain (p=0.007), nausea (p<0.0001), and emesis
(p=0.006), and showed deeper sedation at the end of the rhinoplasty
operations during cast placement (p=0.008). There was a trend towards
better satisfaction with sedation in older patients (p=0.092).
Male patients were less anxious preoperatively both
before (p=0.0027) and after (p=0.069) premedication, and
intraoperatively (with significant patient recall of intraoperative
anxiety). In rhinoplasty procedures, they were more sedated during
osteotomy (p=0.0004) and during cast placement (p=0.035). They also had
less vomiting episodes postoperatively (p=0.021). An average of 90.1%
minimal oxygen saturation (95% confidence interval, 87.8-92.5) was
noticed in all patients.
Midazolam dose was increased when intraoperative
patient anxiety was reported to be high by the surgeon (p=0.011), and it
was higher in patients with less deep sedation at cast placement in
rhinoplasty procedures (p=0.046). Patients who had received a higher
dose of Midazolam reported more intraoperative anxiety (p=0.02) and less
recall of entering the operating room (p=0.0024). Higher midazolam dose
was associated with increased postoperative nausea (p=0.047) and emesis
(p=0.032).
Analgesic intake in the past two weeks tended to be
associated with recall of events from the operation (Chi-2 test;
p=0.05). 29 of 55 patients who had taken analgesics did not recall
events from the operation (53%) versus 36 of 99 patients who had taken
analgesics (36%).
High (7-14 glasses/week) alcohol intake was
associated with slower discharge (p=0.022). In our establishment the
fixed hospital cost In a conscious sedation protocol for blepharoplasty
and rhinoplasty is around 700$ where it is 1700$ in a general anesthesia
setting. This means a 59% cost reduction.
Conscious sedation is an anesthetic technique where
the patient's consciousness level is diminished while maintaining
response to verbal command. Airway protection reflexes, muscle
contraction and thermal regulatory mechanisms are still present thus
preventing aspiration, deep vein thrombosis (DVT), and hypothermia [3].
None of our patients required intraoperative anesthesiologist intervention or an unintended admission. Marcus et al. [1]
reported 15 unintended admissions (out of 300 patients) in their study
using the fentanyl/midazolam conscious sedation protocol, 73% of which
was due to nausea and vomiting. Gart et al. [3]
suggested that although the rate of unintended readmission was low in
conscious sedation patients, high doses of preoperative diazepam
decreased intraoperative midazolam and fentanyl use and reduced the
incidence of postoperative nausea/vomiting. This strategy was found to
decrease the rate on unintended admissions due to nausea and vomiting
from around 1% to 0%.
In our study, the mean recovery time was 196 minutes
(95% CI 181-212). This result is similar to that observed in a study
comparing bolus to continuous midazolam administration (A). The recovery
time for procedures of 120-180 minutes duration was 90-240 minutes.
However, in other studies, intraoperative IV fentanyl rather than
meperidine yielded shorter recovery times (63 minutes) but requiring an
anesthesiologist [6].
90% of patients recalled some events from the
operation while only 10% recalled an intraoperative bad experience.
10.5% of patients in our study reported postoperative nausea and 14%
reported postoperative emesis. In a study comparing conscious to deep
sedation, Hasen et al. [12]
reported a 17% rate of recall of unpleasant intraoperative events in
the conscious sedation group (vs. only 3% in the deep sedation group).
However, both groups had low recall of intraoperative pain, anxiety, and
nausea, and the deep sedation group experienced significantly more
nausea in the recovery room (p = 0.002), at the time of discharge (p =
0.009), and the evening after the operation (p = 0.013). Amnesia of
intraoperative events confers conscious sedation a similar patient
experience to that of general anesthesia. Absence of inhalational
anesthetics and the low dose of narcotics decrease postoperative nausea
and vomiting (PONV) [14].
PONV is often referred to by patients as the most unpleasing issue in
the entire operative experience. It is closely associated with propofol
and with high intraoperative opioid use which favors conscious sedation
over general anesthesia - where propofol and high opioid doses are
employed - and propofol-based deep sedation [3,13].
PONV incidence in benzodiazepine/opioid-based conscious sedation is
reportedly higher amongst women and in the 6-16 years age group
(34-51%), with decreasing incidence with age (14-40%) [14].
Our results fall into these limits with 15.4% of patients reporting a
nausea score of 6 or more on a scale from 0 to 10, with female sex
predisposition, and decreased PONV with advancing age.
In their study on fentanyl/midazolam conscious sedation, Marcus et al. [1]
reported a negative correlation between recovery time and advancing (p
<0.001). Similar results were obtained in our study where older
patients recovered faster (p=0.019), and were discharged faster
(p=0.009).
While general anesthesia remains the corner stone for
most surgeries, it has a 1 to 50,000 fatality rate mainly due to
thromboembolic events [14].
It also presents a risk of malignant hyperthermia and a 30% rate of
post-operative nausea and vomiting despite proper anti-emetic measures,
not to mention increased costs, hospital admissions, preoperative
evaluation time, post-operative recovery time, and complications from
oro-tracheal intubation (sore throat, tooth injury, atelectasis) [1,10,13,14]. On the other hand, conscious sedation decreases the risk of thromboembolic events without DVT prophylaxis [9,15], decreases hospital stay, unintended admissions, and costs, and eliminates the need for a tracheal tube [1,10,15,16].
Many protocols have been described for conscious
sedation in plastic surgery; benzodiazepines are the most commonly used
while propofol, ketamine and barbiturates are fairly found in some
regimens [17-26].
Agents with a short duration of activity/ half-life are preferred and
they are used in small incremental doses while constantly monitoring
patient's alertness, respiratory rate and room air oxygen saturation.
Multiple agents
- propofol, ketamine, and midazolam - possess this property. However,
the advantages that midazolam has include amnestic properties and
reversibility, with increased patient satisfaction and safety,
respectively Propofol and Ketamine lack reversibility and their use by
non-anesthesiologists remains controversial [15].
Midazolam is a short-acting benzodiazepine that provides sedation,
anxiolysis, and antegrade amnesia and these effects are potentiated by
opioid agents. The increased hypnotic effect of midazolam with age and
in females is well documented in the literature [4,5,27]
and is clearly reflected in the results of this study. It should be
noted that the need for sedation is not uniform throughout the
procedure. An initial loading dose is required prior to the infiltration
of the local anesthetic [10].
Once pain suppression is established, the depth of sedation needed
becomes less important. The patient is hence allowed to gradually regain
consciousness during the operation. Another bolus dose is usually added
towards the end of rhinoplasty procedures prior to the lateral
osteotomy to alleviate anxiety secondary to the sounds and vibrations
generated by percussion. This explains why only 10% of our patients
recalled peroperative bad experience while 67% recalled events from the
operation. As for side effects, Midazolam-induced respiratory depression
is primarily manifested by a decrease in respiratory rate while
decreased oxygen saturation only comes next. Therefore, monitoring of
the patient's oxygen saturation at room air but also of the respiratory
rate must take place concurrently [28]. Our technique proved to be safe with an average of 90.1% minimal oxygen saturation (95% confidence interval, 87.8-92.5).
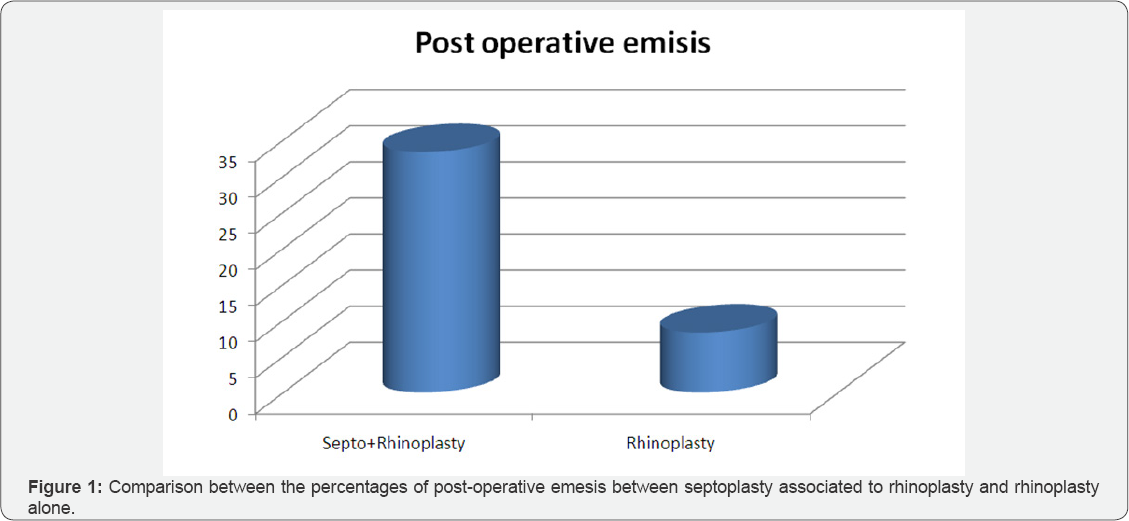
More we can notice in Figure 1 that the septoplasty added to rhinoplasty increases the risk of post-operative nausea by 2.5
folds (Figure 1).
We can also add that rhinoplasty in conscious sedation setting or
general anesthesia if not associated with septoplasty present with
similar post operative emesis and nausea. Finally a key factor to
consider is a reduction of 60% of the patient hospital cost with no
increase in complications and a earlier recovery than general
anesthesia.
Conclusion
This study provides further evidence on the safety
and effectiveness of the IM Meperidine - IV Midazolam conscious sedation
protocol in plastic surgery operations in the one-day- surgery setting.
It has been used at our institution for more than twenty years over
thousands of patients with no major complications occurring. Further
studies are needed to compare the fentanyl/midazolam regimen with this
meperidine/ midazolam protocol with or without dexmedetomidine in terms
of safety, efficacy, and cost-effectiveness.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment