Early Intervention of Cleft Lip and Palate: Current Issues Practices and Protocol-Juniper publishers
Juniper publishers-Journal of Head Neck
Introduction
The most important step towards the treatment of a
child with any disorder is early identification. Early identification
helps in early intervention of a disorder
Early identification
- Is a system of coordinated services
- Promotes the child’s growth and development
- Supports families during the critical early years
- Designed to enhance the development of at-risk infants and toddlers (birth to 3 years of age)
- Prevents speech and language delay
- Provides an access to cheap and best treatment
- Helps the child attend school like any other child.
Major benefits of early intervention
- Early learning forms the basis for complex levels of performance.
- Maximize a child’s developmental capabilities.
- Provides support, instruction and information for caregivers.
- Help parents deal constructively with the grief and stress of having a child with disabilities.
- Parents can find support and assistance to help their child become a more social and independent person.
Need for early intervention of cleft lip and palate
- Babies with cleft palate show deficits in the size and composition of their early sound inventories [1].
- They may reach the canonical babbling stage later than their non cleft peers (Scherer, Williams, & Proctor in 2001).
- The early speech deficits affect later speech accuracy and vocabulary size.
- Before the palate is closed, some babies are attempting to produce stop consonants (Chapman et al. 2003).
Team Members
Pediatrician
They are the first professionals who treat the infant
with various problems. They monitor, record and treat children with a
particular disorder or disease. They are specialists involved child’s
health and care.
Nurse practitioner
Helps in assisting paediatrician, assists baby feed
using prosthesis and tubes when the babies are put in incubators.
Records changes and timely attends to the baby.
Plastic surgeon
Intervenes oral facial defecits surgically by reconstructive surgery. Involved in surgical management.
Pediatric dentist
Helps in correction of teeth in children exclusively as childhood is the period of development of teeth.
Otolaryngologist: Monitors and treats ear nose throat infections as children with facial defects are prone to ENT problems.
Geneticist: Helps in identifying causative genes and is involved in counselling of the family about hereditary syndromes.
Speech pathologist: Plays
major role in monitoring speech and language development and helps in
diagnosis and therapy of speech and language disorders.
Orthodontist: Helps in correcting dentition using prosthesis and braces.
Maxillofacial surgeon: Specialist involved exclusively for
correcting maxillofacial defects by surgical methods.
Social worker: Helps in referral purposes and creating
awareness.
Psychologist: Helps in counselling family and parents go
through grief easily without issues of blame game and other
superstitious beliefs.
Audiologist: Helps in monitoring hearing disorders and its
handicapping conditions.
Early Intervention Program for Children with CLP
CLP is a heterogeneous group of disorder. It can often exist in
isolated form or with multiple disorders and in a syndrome. It is
one of the disorders that are identified at birth. Parents are often
unsure of the impact of the cleft thus they do not know what to
expect from the child. Since it is identified at birth it becomes
easy for planning and executing treatment soon. This requires
proper knowledge for paediatricians to counsel the parents of
the baby the following issues
- The treatment protocol.
- Explaining them about the consequences of delaying the treatment.
- Pre and post operative counselling.
After the 1st and 2nd step the SLP’s and audiologists are
required to play their role in intervention for feeding
management and speech and language problems.
Speech pathologist’s role
SLP’s in coordination with other team members are very
important in providing counselling to the parents regarding:
- Feeding the baby.
- Speech and language stimulation.
- Speech observation.
- Language intervention to facilitate vocabulary development.
- Development of Speech sound accuracy
- Correcting the resonance.
- Improving the speech intelligibility.
Audiologist’s role
Checking hearing status and middle ear functions as
these
children are at risk of developing middle ear infections and
hearing deficits as it would hamper the development of speech
and language problems and even cause delayed speech and
language development. The audiologists must also tell the
parents to observe the child’s responses to sounds and speech as
well as any signs that is expressed by the baby to show some sort of
discomfort in the ear. Also explain them about protecting the
baby from frequent cold and cough.
Areas of Management-Current Issues Practices and Protocols
Feeding
Main factors that are considered important in the
management of feeding includes (Arvedson, 1993)
- Oral motor development
- Availability of nutritious food
- Infant parent relation
Breast feeding
Primary importance:
- Improves mother and child interaction (Tisza and Gumpertz,1993)
- Provides immunity to the child
- Important for healthy development of the child -prevents obesity
- Helps in proper sucking
- Proper development of oral sensory function required for speech and language development (Marques and Martinelli, 1992; Altamann et al., 1994)
- Breast more flexible than rubber nipples and better accommodates the oral cavity so that it occludes the cleft (Biancuzzo,1998)
More advantage in case of presence of cleft lip or palate
because of reduced infections, especially those in middle
ear and prevention of nasal mucosa inflammation caused
by milk reflux (Paradise et al., 1994, Biancuzzo., 1998, 2002,
Crossman., 1998, Aniansson et al., 2002)
Difficulties of breast feeding: (Clarren et al 1987, Chase
et al 1990, Trenouth and Campbell, 1996, Dalben et al 2003,
Thame, 2003):
- Weak suction
- Nasal regurgitation
- Choking
- Insufficient milk production
- Breast engorgement
- Cracked nipple
- Difficulty creating intraoral pressure( Elster,1981, Chase et al 1990)
- Recurrent aspiration for these patients can result in respiratory infections including pneumonia, and even death (Reid et al., 2007).
In a review of feeding intervention study done by Julie
Reid (2003) selected articles were critically appraised using an
evidence-based practice framework to determine the strength of
the evidence underpinning each intervention type for feeding of
the child with cleft. Success of breast-feeding depends on many
factors, including the size of the breast, the size of the baby, and
the severity of the infant’s cleft [2]. Current literature suggests
modifications in the methods of breast feeding.
Bottle feeding
Although breast feeding is considered healthier for the baby,
bottle feeding is also used in cases where breast feeding fails.
Various types of nipple modification can be used to facilitate
bottle feeding. Special kinds of teats are used.
According to Reid et al. (2007), there was a significant
decrease in failure-to-thrive rates for infants with cleft palate
after an early intervention feeding program was implemented.
This program included domiciliary visits, breast-feeding support,
feeding education, and monitoring of growth. Early intervention
can come in many forms including feeding equipment, feeding
techniques, prostheses, and nutrition/lactation advice [3]. Early
education combined with a nutrition intervention protocol can
improve outcomes including: weight gain, feed velocity, and fluid
intake for infants with clefts [3].
Infants with cleft lip ± palate are a significant population
born with congenital defects that will likely require the services
of early intervention providers, including speech-language
pathologists. They are at risk for many health difficulties
including malnutrition that can lead to morbidity and failure
to thrive. They are also at a high risk for laryngeal penetration
and aspiration that can lead to pneumonia. However, evidence
based practice shows that with intervention techniques oral
feeding can be successful and infants can thrive. Until infants
are ready for surgery, care that will enhance their quality of
life is critical for early development. This can be done by using
feeding modifications, or using actual prosthetics. Feeding
modifications can range from consistency modifications given to
the infant, adapting breast-feeding techniques, to nipple shape.
These modifications are vital in assuring that the infant is getting
proper nutrition prior to cleft palate surgery.
Speech and Language Intervention
Another primary goal of early intervention of children with
cleft lip and palate focuses on speech and language development
because these children often show expressive language delay
and phonetic limitation (Chapman & Harding, 1992; O’Garon &
Logeman, 1988). Though speech impairment is due to structural
defect these children show early phonological and language
delays [4] (Blakely & Brockman, 1995, Jocelyn , Penko& Rode,
1996) Hence the treatment focuses on speech and language
stimulation without even waiting for surgical intervention by
using speech and language techniques in order to eliminate
language delays.
Other speech and language problems include the following
[5,6]. Chapman et al. 2003, Salas-Pravana et al. 2003)
- Limited complexity of babbling
- Delayed onset of words and word combinations
- Slow early vocabulary growth
- Limited consonant inventories
- Many sound substitution and omission errors
- Emergence of compensatory articulation errors
It has also been established that potential problems can
be identified in the pre speech stage of development and
preventive work undertaken to promote more normal patterns
of development (Golding-Kushner, 1995, Russel and Grunwell,
1993).
Early intervention programme focuses on the following
aspects
Indirect approach: parents are given target consonants to
model for babbling (Albery& Russel, 1994).
Home based programme: parents are trained to facilitate
and reinforce appropriate patterns in babbling and first words
(Albery& Russel, 1994, Golding - Kushner, 1995).
Games using manipulated vocabulary: In which specific
target words used is effective. (Grundy & Harding 1995, Hahn 1989)
Increasing consonant inventory: (Hardin-Jones, M. ,
Chapman, K. & Scherer, N. J., 2006): The sounds that are least
affected by cleft is first stimulated (e.g., nasals). If the baby
is producing stop consonants, these consonants have to be
reinforced by parents. Parents should avoid reinforcing laryngeal
growls and glottal stops .After palatal surgery, the child begins to
add new consonants (particularly stops) to the inventory. Lack of
growth in the child’s phonetic inventory and persistence of nasal
substitutions or glottal stops are red flags that signal the need for
careful monitoring and early intervention.
Providing a hybrid naturalistic early speech and
language intervention: which gives oppurtuinity to enhance
vocabulary and increase intelligibility which inturn focuses on
both speech and language intervention (Scherer, N. J., 2006)
Using pairs of consonants with whispered vowels [7]:
Keep the glottis open and prevent a glottal stop from occurring.
The child is instructed to over aspirate the consonant-again to
prevent the glottal stop from occurring. As the child demonstrates
success with this whispered production, voicing is gradually
reintroduced for the vowel.
Increasing consonant inventory and vocabulary
simultaneously: For young children, it is often most efficacious
to combine goals for expanding consonant inventory with vocabulary goals. Some considerations are given when choosing
the words to teach children. They are -Small vocabularies are
taken from words used first by typically developing children.
Words must be both functional and fulfill a broad range of
communicative purposes.
Increasing awareness of airflow: In addition to increasing
the child’s expressive vocabulary and consonant inventory, the
SLP may also need to increase some children’s awareness of oral
airflow. Simple blowing toys that offer low resistance can be used
to demonstrate oral airflow, but they should be used sparingly
and considered one of many strategies used to teach sound
production. The blowing activity should follow with a sound
production activity. Although using a blow toy to demonstrate
oral airflow is an appropriate task in therapy, the use of such toys
to “exercise” or strengthen the palate musculature is not.
Goals for early intervention by Judith Crost- Cardomone; October 10, 2008- Exclusive for 0-3yrs
- Early monitoring and speech-language stimulation
- SLP monitors early communicative development and recommends intervention as necessary; counsels parents who are the primary teachers
- Monitor language and speech development and prevent development of compensatory errors
- Monitor VP closure status once palate repair is accomplished.
Early intervention models include
I. Enhanced Milieu teaching [8]- The enhanced milieu
(EM) model has been used to facilitate early vocabulary
growth by focusing on enhancing the early environment
of young children (Hancock & Kaiser, 2006; Hardin-Jones
et al., 2006; Hemmeter & Kaiser, 1994). The EM model
encourages environmental manipulation to facilitate verbal
communication, for example, placing a preferred item out of
the child’s reach to encourage the child to request the item
(Hemmeter & Kaiser, 1994). Specific teaching strategies
are centered on responding to the child during interactions
and prompting the child to use functional verbal behavior
with different techniques, including modeling followed by a
request for verbal imitation or simply a time delay (Hancock
& Kaiser, 2006; Hemmeter & Kaiser, 1994; Kaderavek,
2011). A child needs to verbally imitate to participate in the
imitation activities, but caregivers can implement this model
of intervention in the context of daily activities with children
who have a very limited vocabulary (Hancock & Kaiser,
2006).
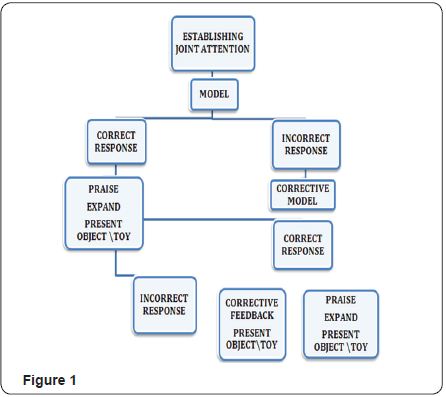
II. Focussed stimulation ( Scherer D’ Antonio & Mc
Gahey,2008)- The parents of CLP were trained to use the FSA
to facilitate the use of target words. The FSA is a procedure
parents can use to increase their child’s vocabulary use.
More you use a word while playing with CLP child, the more
likely the child will use that word (Figure 1).
Enhanced Milieu teaching with phonological teaching (Scherer & Kaiser, 2010)
A set of tools to help facilitate a child’s communication
growth:
- Setting up an interactive context between the adult and child through play
- Noticing and responding to child communication; balancing turns
- Modeling and expanding play
- Modeling and expanding word use
- Using environmental arrangement strategies
- Using prompting strategies to expand language and speech simultaneously
There models can increase vocabulary and clarity of speech
sounds:
- Reduce compensatory articulation
- Train parents to increase exposure to new words
- Provides opportunity for the child to communicate
- Facilitates feedback that can expand language complexity and increase speech accuracy.
Home based EIP services
This method uses readily available materials which makes
intervention more naturalistic and ongoing process rather than
planned process. It makes it easier for parents to see how speech
sound and language stimulation can be centred on the child’s
normal routine. Intervention for treating glottal stops is more
effective through home based programmes. These programmes are effective for babies who demonstrate evidence of language
delays and compensatory articulation. The main goal of early
intervention is to reduce the likelihood of establishment of
abnormal compensatory errors as a habit pattern before it
occurs (Golding& Kaslon, 1981). This method also does not
set aside specific time for training and is facilitated as per
natural interaction process. Stimulation to the chid is provided
throughout the day.
Parental training
Ear training: To make the parent aware of desired response
to be expected from the child and discriminate between normal
and abnormal sound production using tapes and visual cues and
making the parent aware of what is to be expected from the child
and reinforced.
Making the parent aware of the difference between
oral and compensatory articulation and normal speech
and language development: Making use of written materials,
videos speech development milestones charts.
Techniques for stimulating language development:
Parent and child directed speech and motherese with emphasis
on locating objects and requests for naming objects. Engage in
child directed and child centred communication. Other language
stimulation techniques can be used as per situation demands.
Techniques for eliciting correct oral consonant
production and eliminating glottal stops: providing word lists
with target sounds and training the parent to elicit a particular
sound using various techniques. These are to be used even if the
palate is not repaired. Initial target words before palate repair
should be vocalic and nasal loaded with an emphasis on words
that do not begin with vowels as they begin with a glottal stop.
The goal here is to teach alternate word initial strategies. Focus
should be more on pressure consonants and not on hypernasality.
Lip sound play to be used with babies not using their lips. After
palatal surgery, the words should be plosive loaded with anterior
plosives.
Application of behaviour modification techniques: Using
positive reinforcement for correct production and ignoring the
incorrect responses and continuing the training the child by
engaging the child in tasks
Surgical Management and Timing of the Surgery
Timing of the surgery of the cleft lip and palate is linked to
early speech and language development. Early palatoplasty is
said to enhance normal speech production and minimize the
development of compensatory articulation [9]. Since babbling
begins around 4-6 months early surgical intervention becomes
more necessary.
But some oppose to this as they say early repair of hard
palate may affect the mid facial growth and restrict transverse
maxillary development due to scar formation. Some surgeons
prefer to close of the alveolus and lip together as it is easier to
access the alveolus and hard palate before lip closure but this
should not be done in the primary operation stage as it might
interfere with maxillary growth and prefer doing it at the time of
alveolar bone grafting in the later childhood. In such conditions
surgeons prefer to use an obturator for compensating and later
perform the surgery at 4-5 yrs of age (Gilles & Fry, 1921) [10-20].
Some surgeons prefer to close off cleft of the lip during the
neonatal period so that the parents do not have to suffer the
distress of looking after the baby stigmatized in this way (Desai,
1979). But majority of the surgeons wait until the infant is 3-6
months. One- stage palatoplasty procedure for simultaneous
closure of both hard and soft palatal defects. Is not performed
until 1yr to 18months of age as it has more advantages and
repeated surgery It also indicated better speech and language
development (CSAG,1998, Somnerlad et al, 1997).
In rare cases, pre surgical orthopaedics may be required
(0-3months). In this the surgeon seeks to obtain optimal function
and appearance and avoid the need for extensive revisionary
surgery by using proven surgical techniques that result in
minimum scarring. In some cases, it can help the surgeon unite
with minimum stress to the tissue.
- Reposition of severely displaced maxillary segment
- Reduced width of very wide cleft
- Improve symmetry of nose and jaw
The timing of the surgery of the lip and alveolus is dependent
on the time it takes the orthodontist to move segment of the
alveolus arch into proper alignment. This is done by 3-4 months.
Palate repair to eighteen months general communication can
be observed. Progress includes increase in labial and lingual
articulation (p, m, l) and development of oral plosives (p, b,
t, d, k, g). If oral pressure consonants fail to develop it can be
due to several factors but still it is important to identify this
atypical pattern as soon as possible for proper management.
Focus should me on voiceless plosives (Russel & Grunwell, 1993;
Mouset & Trichet 1985).
Despite controversies, majority of the studies have suggested
that earlier surgery was associated with better speech and
language development (Holdsworth 1954, Jolleys 1954, peer,
1961, Cleveland and Falk 1970, Evans and Renfrew 1974, Dorf
and Curtin, 1982, 1990, Randall et al 1983, O’ Gara and Logemann
1988, O’Gard et al. 1994, Rohrich et al, 1996, Marrinon et al 1998,
Ysizio et al , 1999, Hardin and James & Jones 2005).
Other advantages include:
- Better articulation ( Evans & Renfrew 1974, Kaplan et al. 1974, Dorf and curlin 1982, 1990, Rohrich et al 1996, Ysunza et al 1998)
- Less compensatory articulation ( Dorf and Curtin 1983, 1990, Ysuzahn el al 1998)
- Normal resonance ( Evans and Renfrew 1974, Rohrich et al 1996, Hardin Jones and Jones 2005)
- Less need for secondary surgery ( Cleveland and Falk, 1970).
Conclusion
Early intervention is proved to be beneficial in case of cleft
lip and palate for better speech and language development.
Timing of the surgery continues to be controversial, thought
most surgeons prefer doing it as early as possible. Brest feeding
is more preferred by mothers and in rare cases bottle feed is
required.
To know more about Journal of Head Neck please
click on :
To know more about Open access Journals
Publishers please click on : Juniper Publishers

Comments
Post a Comment