Dysphagia: Approach to Assessment and Treatment-Juniper publishers
Juniper publishers-Journal of Head Neck
Dysphagia is a medical term used to describe a
swallowing disorder. It may refer to a swallowing disorder involving any
one of the 3 stages of swallowing: oral, pharyngeal, esophageal. It is
not a primary medical diagnosis, but a symptom of a disease, &
therefore is described most often by its clinical characteristics.
Dysphagia is delay in or misdirection of a fluid or solid bolus as it
moves from mouth to the stomach. Delay in or misdirection of the food
bolus may interfere with functional oral intake.
The nature of dysphagia
Aspiration occurs whenever food enters the airway
below the true vocal folds. Aspiration can occur before, during, or
after the swallow.
Aspiration before the swallow
Aspiration occurs before the swallow in the case of a
delayed or absent swallow initiation. It may also be the result of poor
tongue control, which allows food to trickle into the pharynx while the
patient is still chewing. Apparently, a “neurological override” exists
which prevents the initiation of the swallow while one is still chewing
[1].
Aspiration during the swallow
Aspiration occurs during the swallow when the vocal
folds fail to adduct or the larynx fails to elevate. (Remember that this
type of dysphagia is uncommon. Only 5% of dysphagias involve problems
with airway closure).
Aspiration after the swallow
Aspiration can occur after the swallow in several
different circumstances: The patient may pocket food in the oral cavity.
Later, when he or she lies down to sleep, the food will fall down into
the airway. Food may get stuck in the pharyngeal recesses. This happens
to everyone, but someone with a normal system would realize that the
food was there and swallow again. A CVA or TBI patient may have a
sensory impairment and allow the food to drop into the larynx. Due to
reduced laryngeal elevation, food may remain on top of the larynx
(Logemann, 1989).
Signs & symptoms of dysphagia
Early identification and treatment (Tx) may help
avoid adverse medical complications such as under nutrition or
respiratory infection. Because a variety of medical specialists can be
involved in the care of the patient with dysphagia, all must be capable
of detecting the signs & symptoms characteristics of dysphagia. Some
symptoms may be overt, such as those in the patient who coughs while
eating, where as others may not be overt, such as those in the patient
who may not have a swallowing complaint but comes to the swallowing
specialist with a history of unexplained pneumonia.
A radiographic evaluation of swallowing may reveal
that food or fluid is silently entering the air way during swallow,
resulting in aspiration.
Symptoms of dysphagia: symptoms are
usually are defined as any perceptible change in bodily function that
the patient notices. This change eventually leads the patient to seek
medical help when it causes pain or discomfort or negatively impacts
his/her life style. Some people have adverse medical symptoms &
ignore them until the severity of their problem significantly affects
their physiologic or mental health. Others seek immediate medical
attention. Both groups may be diagnosed with a disorder that is similar
in type & severity.
Patient description: the physical examination of a
patient with dysphagia may begin by asking him or her to describe the
symptoms. Because dysphagia often is secondary to neurological disease
that also may compromise communication skills, not all patients can
provide a report of their symptoms.
Because of cortical deficits, others may give
unreliable or scant information. They make changes in their eating
habits to accommodate their symptoms, such as chewing food more finely
or eliminating troublesome items from their menu. Others know that they
are having difficulty swallowing but have a difficult time describing
the specifics of their symptoms. Often it is difficult for them to
remember how long those symptoms have been apparent.
This may be due to the inherent flexibility of the swallowing
tract to accommodate changes in function. For patients who are
able to communicate symptoms of their dysphagia, a detailed
description may be useful in helping establish a diagnosis.
Detailed descriptions also may be used to help the examiner
focus on the types of diagnostic tests that may be most useful in
delineating the source of the patient’s complaint. Some clinicians
find it useful to explore a patient’s dysphagic symptoms by
questionnaire. This method may help ensure that all relevant
questions relating to the patient’s symptoms are addressed by
the examiner. It also gives the patient a chance to think carefully
about his/her symptoms before responding.
Obstruction: one of the common complaints from dysphagic
patients is that food or fluids “gets stuck”. Most often, they
report that the sticking sensation is in the throat or esophagus.
Some patients do not use the word stuck but may use the word
“fullness”. When they localize the feeling of obstruction to the
throat, they often describe their complaints as “a lump in the
throat” when eating.
The medical term for this feeling is globus. Some physicians
have used the term globus hystericus to describe this sensation,
because it was once thought usually that the description of lump
in the throat usually was associated not with organicity, but with
symptoms of hysteria.
Liquids vs solids: Patient may report a change in their
dietary habits that is associated with perceived dysphagia.
Those who complain of the globus sensation often have more
difficulty swallowing solids than liquids. Patients with solid food
dysphagia are more likely to have disorders of esophageal origin;
whereas these who complain of dysphagia for liquids are more
likely to have oropharyngeal dysphagia. When patients complain
of choking on liquids or solids, a more pharyngeal focused cause
is suggested. Whereas those who report dysphagia for liquids &
solids without choking episodes may have a more esophageal
focused cause.
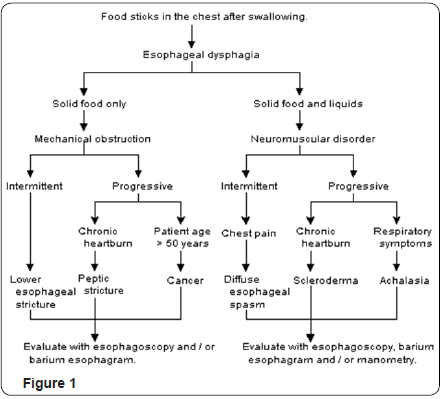
Gastroenterologists who support the esophagus as the source
of dysphagia may use a decision tree such as the one presented
below to assist in diagnosis. Such a decision tree has not been
validated against a large number of patients with confirmed
diagnosis; however, the concept is useful because the symptoms
related to the represented diseases are well known, & the no. of
potential causes for esophageal dysphagia is limited.
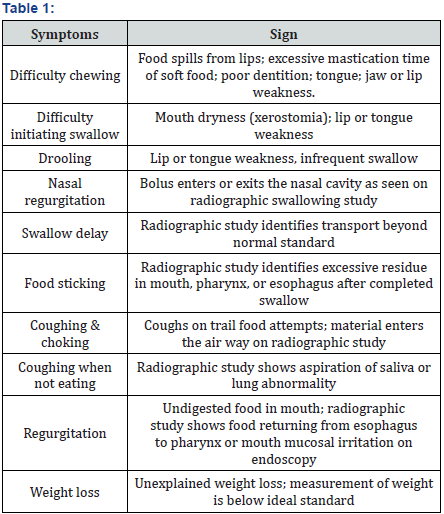
Symptoms & signs that may related to many disease entities.
Thus using a decision tree approach based on patient complaints
does not provide enough precision to help the clinician establish
a diagnosis for Patient with oropharyngeal dysphagia. Gastro
esophageal reflux: some Patient complain of episodes of gastro
esophageal reflux (heart burn) associated with their complaint
of dysphagia. Some Patient describe pain or fullness in the chest
associated with their reflux.
Others may have reflux & dysphagia but may be unaware that
they have reflux because the overt symptoms of chest pain or acid
taste are not present. Not all Patients describe episodes of reflux
unless questioned by the examiner, because they may not relate
their episodes to their dysphagia. This is particularly true when
Patient complain of globus sensation in the neck, because they
might think that reflux in the esophagus could not be related to a
problem in the throat. Eating habits: a Patient’s report of changes
in his/her eating habits may signal the presence of dysphagia, its
level of severity, & its psychological impact.
Complaints that elimination of specific food items from the
diet, such as liquids or solids or items that are sticky or crumby,
may help the examiner focus the evaluation. Excessive chewing
of solid food to avoid a sticking sensation may be more consistent
with esophageal disease Vs the pharyngeal focused complaint
that liquids always seem to come back through the nose. People/
patients who report excessive time to finish a meal often have
dysphagia that requires careful evaluation. Patients who report
that they no longer feel comfortable eating in a restaurant
because they have to regurgitate or choke should be examined
with care. Patient who have experienced marked weight loss
or who no longer enjoy the pleasures of eating probably have
dysphagia that has reached a high level of severity.
Signs of dysphagia: signs are objective measurements or
observations of behaviors that people elicit during a physical
examination. In a dysphagic patient who is cooperative, this
measurement entails an examination of the cranial nerves
relevant to swallowing. Some signs are seen during observation
of the Patient eating. Signs & symptoms may overlap. Example
A Patient may complains have liquid going into the nose &
food sticking. Both may be seen by the examiner on the video
fluoroscopic swallowing study.
- The physical evaluation of a Patient may reveal signs that are consistent with dysphagia, such as
- Drooling from the lip or tongue weakness
- Poor dentition
- Loss of strength or range of motion in the tongue, jaw or velum
- Poor strength or coordination may result in choking on liquids during test swallows or in lack of bolus flow
- The pt’s cognitive status may impact swallowing eg. Failure to chew, talking while swallowing, inattention to the feeding process
Patient who are hospitalized may have more overt medical
signs, such as
- Feeding tubes that are already placed
- A tracheostomy tube
- Poor dentition
- Respiratory congestion after eating
- Requirement of excessive oral & pharyngeal suctioning
- Eating refusals
- Under nutrition & muscle wasting
- Inability to maintain an upright feeding position
- An endo tracheal tube
- Regurgitation of food
The process of evaluation begins with case history, clinical or
bedside swallow examination and the instrumental examination.
In many assessment protocols, the case history and bedside
swallow evaluation are combined. They provide greatest
amount of information on the patients eating behavior, language,
cognition and oromotor function.
Screening procedure
Screening procedures provide the clinician with some
indirect evidence that the patient has a swallowing disorder. It
tend to identify the signs and symptoms of dysphagia such as
coughing behaviors, history of pneumonia, drooling, chewing
difficulties or the presence of residual food in the mouth.
Screening procedures are generally performed at the patient’s
bedside or in a home or school environment and provide the
clinician with increased evidence that the patient needs an in
depth physiological assessment.
Screening procedures provide the clinician with some
indirect evidence that the patient has a swallowing disorder. It
tend to identify the signs and symptoms of dysphagia such as
coughing behaviors, history of pneumonia, drooling, chewing
difficulties or the presence of residual food in the mouth.
Screening procedures are generally performed at the patient’s
bedside or in a home or school environment and provide the
clinician with increased evidence that the patient needs an in
depth physiological assessment.
In adults, the Burbe Dysphagia Screening Test (BDST) is used
which consisted of a seven items. It checks the presence of one
or more items in the test results in failure and then referral for
a complete bedside swallow evaluation. The screening items are
- Bilateral strobe
- Brain stem stroke
- History of pneumonia in acute phase strobe
- Cough during 303 water swallow or associated with feeding
- Failure to consume one half of meals
- Prolonged time required for feeding
- Non-oral feeding programs.
This test is reported to highly valuable in identifying patients
are risk for swallowing problems
Bedside examination
It is designed to define the function of patients lip, tongue,velopharyngeal region, pharyngeal walls and larynx as well as
his/her awareness of sensory stimulation. The physiology of
some of these structures can be easily assessed at the bedside,
while others can only be examined accurately in radiographic or
other instrumental study. It consists of following examination.
Review of patient’s medical chart
- Prior to entering the patients room, the clinician should carefully review the patients medical chart, focusing particularly on the medical diagnosis, any prior or recent medical history of surgical procedures, trauma, neurological damage as well as patients current medications.
- After defining medical diagnosis, the clinician should immediately consider what physiologic or anatomical swallow disorders that are typical of that diagnoses.
- History of any respiratory problems should also be identified, including need for mechanical ventilation or tracheostomy tube, the conditions under which they were placed (emergency/planned).
- Prior history of GI dysfunction should be noted.
- Prior history of dysphagia from earlier stroke or head injury should be high-lightened even if the patients or his/ her family indicates that the patient returned to oral intake with no apparent difficulty.
- Medical chart should reveal the patients current nutritional status and the presence of any non-oral nutritional support such as naso-gastric tube.
- Clinical should also be able to identify the patients general progress as well as prognosis from chart review.
Oromotor examination
It begins with the examination of anatomic structure of oral
cavity including its symmetry and presence of any scar tissue
indicating surgical/traumatic damage. The oral examination
should note the presence and status of oral secretions, especially
the pooling of secretions or excessive dried secretions. In general,
the locus of excess secretions in the oral cavity indicates the
areas of lesser lingual control or injury. Oromotor examination
should then proceed to examination of strength, range of motion
and coordination of the lips, tongue and palate for speech and
non-speech tasks as well as observation of lingual function and
lip closure while the patient produces spontaneous swallows,
clinician notes down the frequency of spontaneous swallows.
Respiratory support
Respiratory support should be defined by counting the rate
of breaths per minute. Patients should be asked to hold their
breath for a total of 1 sec, then 3, 5 and 10sec and the clinician
should observe whether this behavior creates any respiratory
distress. Duration of breath hold should be increased as tolerated
by the patient. This determines whether the patient can tolerate swallow maneuvers or other therapy procedures that increase
the duration of apneic or airway closed period during the
swallow. Generally patients need to hold the breath of 5 seconds
to use swallow manneurs comfortably. The patients coordination
of swallowing and respiration should be observed.
Prolonged phonation
Prolonged phonation on the vowel/o/ should also be
examined in terms of both vocal quality and respiratory control
used. Clinician should then check whether the patient is able
to take an easy inhalation followed by a slow drop of chest and
inward motion of abdomen to produce a prolonged vowel on
sustained phonation of at least 10 seconds.
Gag reflex
This is to examine the pharyngeal wall motion as part of
the motor response for gag. The pharyngeal wall motion during
the gag should be symmetrical. Any asymmetry-unilateral
pharyngeal wall paresis.
Laryngeal examination
- Series of voluntary tasks will be tested which are as follows:
- Vocal quality on prolonged /a/ (hoarse, gurgley)
- Strength of voluntary cough
- Strength of throat clearing
- Clarity of /h/ and /a/ during repetitive /ha/
- Pitch range (slide up and down scale)
- Loudness range
Cognitive and language characteristics: Through all
oromotor testing, the clinician will be examining the patients
general behavioral level, ability to discipline his/her own
behaviour, and focus on tasks, impulsiveness, ability to respond
to commands, etc, should also be tested.
Optimal protocols: De Pippo et al. have proposed other
options in place of bedside swallow evaluation. They found that
cough or voice change during or directly after drinking 303
of water was sensitive and valid screening tool for aspiration
following a stroke. It should be remembered that the clinical
swallow assessment with water should be tried only after the
findings from patient history and oropharyngeal examination
should be taken into account. Patients unable to tolerate their
secretions, who have limited attention such as those after a
severe stroke or who resist for some other reason may not be the
candidates for clinical swallow test.
Dysphagia screening: Prior to
bedside swallow, use of
dysphagia screening test may be appropriate. This is usually
done by speech language pathologist but may also be done by
a nurse trained in the procedure. Two such screening tests are
the Burbe Dysphagia Screening Test (BDST) and the screening
test proposed by Odderson & McKenna. The BDST consists of a seven
item test. Presence of one or more items in the test results
in failure and then referral for a complete bedside swallow
evaluation.
The screening items are
- Bilateral strobe
- Brain stem stroke
- History of pneumonia in acute phase strobe
- Cough during 303 water swallow or associated with feeding
- Failure to consume one half of meals
- Prolonged time required for feeding
- Non-oral feeding programs.
These 2 tests are reported to highly valuable in identifying
patients are risk for swallowing problems.
Dye test
Also known as Blue dye test may be used to determine the
presence of aspiration in a tracheostomized patient. A few drops
of methylene blue or vegetable coloring are placed in the mouth,
tracheostomy cuff is deflated, and the tracheostomy tube is deep
suctioned for secretions that may have been resting on or above
level of cuff. The patients tracheostomy tube is deep suctioned
and looking for evidence of dyed material in airway. This may not
detect trace amounts of aspirated materials.
Auscultation: Chest and cervical
Placing a stethoscope over various parts of airway provide
indirect evidence of aspiration. Through this, he can listen to
airflow during normal breathing, swallow sound. It determines
whether other tests are needed.
Clinical Swallowing Examination (CSE)
The clinical swallowing examination allows a circumscribed
exploration of patients muscle function, sensation and airway
protective functions. This CSE allows the clinician to develop
management program for the patient and to determine the
necessity of further instrumental assessment. The clinical
swallowing examination protocol includes the following:
CSE 1 Mental status
We know that there is interdependence between safe swallow
function and cognitive and behavioral factors such as attention,
memory, judgement, reasoning, orientation and sequencing
skill. In patients with head injuries, the frequency of swallowing
disorders was found to decrease as patient’s scores on level of
cognitive function scale improved [2].
During the interview, clinician should be vigilant for
indications of reduced mental function.
- Are the clothes clean or blotched with food particle? (Subtle questions)
- Is there an evidence of appropriate attention to cleanliness and hygiene? (Subtle questions to cleanliness and hygiene? (Subtle questions).
- Is the individual attending to the questions and answering appropriately?
- Is there a drift during the session?
- Is the caretaker/spouse acting as a surrogate in the interview without invitation…… etc
Many scales have been developed for measuring and
monitoring mental status eg.
a. Glassgow coma scale. It is scored for 3 behaviors, eye
opening verbal response and motor response. The score
range from 3 (severe coma) to 15 (full awareness)
b. The Ranchos Losnmigos scale.
c. All these scales tell us about degree of cognitive
impairment.
CSE 2 Speech/Articulation
Here the clinician makes a gross determination of
a) Precision of articulation i.e. speech intelligibility, look
for the % speech intelligible
100% - normal
>50% - moderate
35 – 50% - severely affected
< 35% - very unintelligible
b) Rate – normal; slow; accelerated
c) Predominant error- Check whether distortion/
omission/substitutions present. Distortions are more likely
to be present in neurogenic speech disorders.
CSE 3: Respiratory function
Here the respiratory subsystem is assessed which includes –
a) Volitional cough: Ask the patient to take a breath and
produce as great a cough as possible. Check whether he is
able to cough or not if not see for the presence of forced
expiration, throat clearing or hawking. (Hawking: audible
effort to force out the phlegm from throat).
Also check for productive cough (transport of material from
lower airways.
Check for loudness (normal, weak/audible or very weak/
inaudible).
b) Sustained expression while counting: Ask the patient to
inhale as deeply as possible and with a single breath, count
as high as you can. The score is derived from the number
reached when patient counts aloud on a single exhalation
after maximum inspiratory effort.
c) Index of pulmonary dysfunction: Smeltzer, Skurnick,
Toroiano, Cook, Duran and Lavietes (1992) employed an index sensitive to pulmonary dysfunction. The possible
range of scores 4 (normal maximal expiratory pressure to11
(poor maximal expiratory pressure) [3,4].
CSE 4: Voice/resonance
For assessing this, clinician will rely on connected speech
and check for normal/hoarse/ harsh/hypophonic/ aphonic or
wet dysphonic/hypernasal.
CSE 5: Position
Clinician will observe the patients habitual body and head
position and examine the patients adaptations or apparatus
used to assist in support. The clinician then will attempt to elicit
alterations in body and head positions.
Body position- Leaning with self support.
- Supported by apparatus.
- Reclined.
- Flexion.
- Extension.
- Head turned to left/right
Eliciting changes in position during the clinical examination
allows the examiner to probe for the patients capacity to
change the position or posture later in assessment process.
Repositioning the head and trunk has been shown to cause
changes in biomechanics of swallowing.
CSE 6: Lip sensation/strength/seal
a. Ask the patient to close his/her eyes and respond
either verbally or by raising a finger or hand in response to
stimulus placed on the lip and its marging (light momentary
brush over).
b. Checking drooling is present/not.
c. Note down the habitual oral position ie open/closed.
d. Lip strength can be assessed by asking the subject to
purse his/her lips with as much pressure as possible and ask
him to lift the upper and lower lip with tongue blade along its
entire length.
CSE 7: Mouth opening
a. The patient is asked to open his mouth as widely as
it will open and see whether it is normal/reduced mouth
opening (approximate mouth opening: 1 cm).
b. This is assessed because patients with small mouth
openings may have great difficulty placing even small volumes of food in their mouth. The amount of time and
effort need to take in enough food to maintain nutrition lead
these patients to abandon oral solid foods in favour of liquid
diets that are easily consumed by straw.
CSE 8: Muscles of mastication
Masseter and temporalis: They act to move the mandible to
a closing position. With the jaw muscles relaxed, ask the patient
to clench down on a tongue, blade placed along the length of the
molars on the right or left side of oral cavity. Palpate and note
down the bulging and firmness.
Lateral and medial pterygoid: Check for protrusion and
lateralization by applying resistive pressure on the other side
with other hand.
Check for pain while performing the above mentioned tasks,
see whether the pain is unilateral or bilateral also.
CSE 9: Dentition and periodontum
Clinician assesses the patients dentition prosthetic dentition
and gingiva. The equipment needed includes a penlight, gloves
and tongue depressor – we have to make a note of existing teeth
and missing teeth in the tooth chart - also indicate the condition
of existing dentition.
Removable prosthetics: While inspecting the mouth, make
note of removable partial/complete dentures. A partial denture
replaces one or more teeth in one arch. A complete denture
replaces most or all of the teeth in an arch. Indicate where the
prothesis are in place and note their condition with the patients
mouth wide open, grasp the denture and tug on it to determine
firmness – check for the presence of food particulate or plague
on the surface of the denture.
CSE 10: Salivary flow/appearance of oral mucosa
Check whether the salivary flow is normal or any
hyposalivation is present.
Check for the appearance of oral mucosa i.e. surface of the
tongue appears severely dry, tongue with cracks and fissures etc.
CSE 11: Oral/pharyngeal gag
Have the patient open his/her mouth as you probe the
surface of the tongue, faucial pillars and posterior pharyngeal
wall. Initially apply light touch and probe for the response. If no
response, apply enough pressure.
CSE 12: Tongue movement/strength
- Request the patient to open his/her mouth and observe the tongue at rest and during protrusion. Check whether the tongue is normal/atrophied/deviated/dyskinesia.
- Also check for nasal respiration. thro lips. This task tests the posterior seat of oral cavity.
- Tongue strength should be tested with isometric exercises. See whether strength is normal/reduced.
- Tongue range of motion can be checked by requesting the patient to move the tongue tip along the entire length of maxillary and mandibular buccal sulci. Also ask the patient to stroke over the surface of hard palate.
CSE 13: Velar elevation
Ask the patient to say or yawn and check for velar elevation.
CSE 14: Volitional swallows/laryngeal elevation
- Place the ring, middle and index fingers along the entire surface of throat with the index finger in the superior position. Situate your finger so that the thyroid notch is nestled between ring and middle fingers. Here index fingers should be resting on suprahyoid muscles. Request the patient to swallow with the fingers lightly resting upon the suprahyoid muscles. There may be a moment of delay as the patient collects saliva within oral cavity and prepared to swallow.
- Patients with xerostomia – no enough saliva to initiate dry swallows.
- Apraxia – no coordinated swallow
- Cognitive impairment – unable to swallow on common.
- The sublingual musculature pull away from index finger as the suprahyoid muscles contract. During elevation, the thyroid notch should move to a point above the middle finger and at the apex of the swallow, may come in contact with the inferior margin of the index finger. A swallow following this pattern is normal.
CSE 15: Food and liquid swallows
The clinician will elicit swallows by presenting food and
liquid of varying volumes and consistencies to the patient. The
clinician will observe and record signs and symptoms that are
exposed during the session. As a basic guideline, the clinician
should hold safety as the highest priority. Clinician should be
sure of the following:
- Alertness
- Cough: strong cough, weak cough
- Accordingly we can introduce any material in the patients mouth.
- Order of presentation should be taken into account. The initial delivery should be of and consistency that will be the easiest for the patient to consume. Graded activities should be done eg. Slowly increasing the volume.
- Enter the maximum amount of food or liquid presented with a particular material (listing the volume is also important).
- Timing of the onset is dependent on the materials presented with longer period necessary as the hardness of the food increases. The elapsed time should begin as the food enters the mouth and end as the larynx elevates for pharyngeal swallow.
- Clinician should count the number of swallows per bolus delivery by recording the number of elevations of the larynx. When multiple swallow occurs, the clinician should query the patient regarding the presence of food sticking. If able, have the patient point to the perceived location of the residue. Accordingly instrumental techniques is indicated.
- Oral signs: Clinicians should look inside the patients oral cavity following each food presentation in those patients who report oral stage difficulties. Attention should be given to all cervices and pockets where food can get accumulated.
- Airway signs – note the presence of wet dysphonia and frequent cough (liming and strength).
Instrumental Techniques for the Study of Swallowing
Introduction
A number of imaging and non-imaging instrumentation
procedures have been used to study various aspects of normal
and/or abnormal swallow physiology. Each procedure provides
some pieces of information on oropharyngeal anatomy or
swallow physiology. It is important that the clinician be
familiar with the types of information, each procedure provides
information about swallowing and basic methodology for each
procedure. These instrumental procedures include
- Imaging studies.
- Non-imaging studies.
Imaging studies
Several technologies can be used to image the oropharyngeal
region which include ultra sound, video endoscopy, video
fluroscopy, pulse oximetry, scintigraphy, CT and MRT,
esophagoscopy/gastroscopy.
Ultra sound
Ultra sound uses high frequencies sounds (>2MHz) from a
transducer held or flexed in contact with skin to obtain a dynamic
image of soft tissues. As ultrasound does not penetrate bone, its
use is limited to the soft tissues of oral cavity and parts of the
oropharynx. Here a handheld transducer is placed submentally
and is rotated 90 degrees. It is used to observe tongue function
and to measure oral transit times as well as motion of hyoid
bone. Real food can be used here.
Videoendoscopy (FEES)
It has been used increasingly in recent years to examine the
anatomy of oral cavity and pharynx and to examine the pharynx
and lx before and after swallowing. First described by Langmore
et al. It requires the passage of a fiberoptic laryngoscope into nares, over the velum to a position above the epiglottis. After
placing the endoscope, examiner notes the anatomic structures
and observes the functions of the velum, epiglottis and larynx
using sustained phonation or repeating coca cola. Trial dry
swallows are prompted to elicit laryngeal elevation.
Specific amounts of liquids and food consistencies treated
with food dye are viewed as they pass the pharynx and larynx.
During the time of airway closure, swallow cannot be visualized
as the pharyngeal walls contract over the bolus, collapsing the
lumen over the endoscope (whiteout phase). Monitoring of the
bolus is only possible before and after pharyngeal swallow.
Video camera monitors the bolus as it enters the view from oral
cavity to pharynx.
It can be used to determine sensory dysfunction in dysphagic
patients. To perform the test, an air pulse generator is used
to send a pulse of air through a port in a specially designed
flexible nasopharyngoscope. Air pulses can be delivered to the
supraglottic larynx and pharynx areas. Using a calibrated puffs
of air, sensory thresholds can be determined using one of the
psychophysical testing methods. The twitching response of the
mucosa suggests the sensory awareness of stimulus.
Scintigraphy
It is a nuclear medicine test in which the patient swallows
measured amount of radioactive substance (technetium-99m)
combined with liquid/food. A special gamma camera records
images of the organs of interest over time. This can also be
used to identify aspiration, quantify aspiration over short/long
periods of time. It can also be used to calculate transit time and
residual pooling of a bolus before and after treatment. If there is
no aspiration and reflux is suspected, the patient is rescanned
every 15-20 min for several hours to detect reflux.
Pulse oximetry
A relatively new approach to monitor swallowing and
possibly detecting aspiration is pulse oximetry. It is based on
the principle that reduced and oxygenated hemoglobin exhibit
different absorption characteristics to red and infrared light
emitted from a finger/ear probe. Pulse oximetry measures
oxygen desaturation of arterial blood, a condition which is
thought to occur as a result of aspiration. It is non-invasive,
simple may be repeated often but does not provide diagnostic
information to formulate treatment plans. It offers information
regarding presence and possibly severity of aspiration.
Videofluroscopy
Because swallow is a dynamic and rapid process,
videofluroscopy is particularly well suited to the study of this
physiologic function. The term cookie swallow has been in the
past but this does not describe the procedure adequately.
Modified barium swallow has two purposes: To define
the
abnormalities in anatomy and physiology causing the patients
symptoms. To identify and evaluate treatment strategies that may
immediately enable the patient to eat safely. Baruim swallow test
can be used to examine oral transit times, structural competence
of oesophagus, particularly lower two thirds of oesophagus very
well.
Test
Under fluoroscopic observation, controlled by the radiologist,
the patient ingests barium coated boluses or liquid barium of
varying consistencies.
Placement of food in the patients mouth: Generally food
is placed in the patients mouth on a disposable plastic spoon.
If a patient has a bite reflex, a heavier plastic spoon is more
appropriate. For infants, bottle and nipple may be used.
Type and amount of material used: At least three
consistencies of material are used in the modified barium
swallow to investigate patient complaints of variable swallowing
ability. Thin liquid barium (as close to water as possible), barium
paste (chocolate pudding mixed with esophatrast) and the
material requiring mastication (a cookie coated with pudding
mixed with esophatrast). At least two swallows of each material
are given in following amounts: 1ml 3ml, 5ml, 10ml and cup
drinking of thin liquid; 1/3 teaspoon of pudding and a fourth of
a small Lorna Roone Cookie coated with barium [2]. Volume of
liquid is increased until or unless patient aspirates.
Positioning the patient: Often the most difficult and time
consuming part. No. of chairs for positioning patients during the
radiographic study have been designed. A patient who is mobile
and able to sit without a backrest can be seated on the horizontal
platform attached to fluoroscope table and raised/lowered to
desired height. Most machines are fitted with handles so that
the patient can stabilize his/her position. Some fluoroscopy
machines will not accommodate wheel chairpersons or persons
on cart. If permitted, they are positioned on a cart with the head
of cart elevated to at least 90 angle.
Focus of fluoroscopic image: The fluoroscopy tube should
focus on lips anteriorly, hard palate superiorly posterior
pharyngeal wall posteriorly and the bifurcation of the airways
and oesophagus inferiorly. Many fluoroscopy machines permit
image magnification.
Measures and observations to be made: lateral view:
This permits a number of measures and observations critical to
the identification of patients anatomic/physiologic swallowing
disorder. It helps in measuring oral, pharyngeal and oesophageal
transit time. This permits identification of the location of the
bolus as it moves along upper aerodigestive tract from anterior
superior to posterior inferior. It permits the analysis of patterns
of lingual movement, estimate of amount of material aspirated
per bolus, as well as the reason for aspiration. The timing of
aspiration relative to triggering of pharyngeal swallow is also
best examined.
The eight step scale maybe quite useful to monitor changes in a patients ability to control aspiration material.
- Does not enter airway
- Remains above folds / ejected from air way
- Remains above folds / not from air way
- Contact folds / ejected from air way
- Contact folds / not ejected from air way
- Pass below folds /ejected into lx or out of air way
- Passes below folds /not ejected despite effort
- Passes below folds / no spontaneous effort to eject.
Posterior anterior view (P-A view): P-A view is helpful in
looking at asymmetries in function, particularly of pharyngeal
walls and vocal folds and in viewing the residual material in the
valleculae and in one or both pyriform sinuses. It provides vocal
fold movement picture too.
Other radiographic tests for dysphagia
Upper gastro intestinal series: The single contrast
esophagram study fills and distends the lumen with thin liquid
barium. Intrinsic mural irregularities and masses and extrinsic
impressions are visible. An air contrast study provides the same
information but allows a more detailed view of mucosa. For an air
contrast barium study, the patient ingests effervescent crystals
followed by thick barium. A barium swallow has both dynamic
and static components. The dynamic portion, fluoroscopy can be
recorded on tape (video fluoroscopy cine radiography) for later
review. The static portion is recorded on a series of rapid still
frames.
The barium swallow can identify intrinsic and extrinsic
pathology. Intrinsic abnormalities include tumors,
cricopharyngeal dysfunction, aspiration of barium into airway
or reflux into nasopharynx, diverticulas webs and esophageal
dysmotility. Extrinsic masses such as cervical osteophytes and an
enlarged thyroid gland maybe visualized directly or suspected
by their effect on the barium column.
The subjective location of dysphagia does not always
correspond to anatomic location of pathology. Therefore, the
barium study when used to evaluate dysphagia should extend as
low as the gastric fundus or cardia. The upper gastroesophageal
series evaluates the stomach and relaed areas. Obstruction or
dysfunction of these areas may cause or contribute to esophageal
dysfunction (eg. GERD). Thus the transitional barium swallow
evaluates the upper aerodigestive tract between oral cavity or
oropharynx and gastric fundus or cardia. It is not intended to
identify swallow dysfunction or to dictate treatment as in the
modified barium swallow.
Computer tomography and magnetic resonance imaging:
They are used to delineate the anatomy of a particular region of
the head, neck or other components of the upper aerodigesture
tract. The most common use is to identify a site of lesion such as cerebrovascular accident within the central nervous system or
to delineate the extent of an intra/extra luminal space occupying
system. In general, CT offers direct axial and coronal images that
better define bony anatomy.
MRI better delineates the soft tissue in saggital, coronal
and axial planes but takes longer to complete the images and
thus is prone to motion artifact. High speed MRI such as fast
low angle shot (FAST) or echo planar imaging, has allowed a
dynamic analysis of the pharyngeal phase of swallowing that
was impossible with conventional MRI. The pharyngeal oral
cavity, laryngeal lumen and musculature can be evaluated during
motion, allowing the assessment of swallowing mechanism.
During FAST MRI, images are obtained as a bolus containing
contrast substance is so allowed. Here temporal and spatial
resolution is poor, but no exposure to radiation.
Non imaging techniques: They provide a variety of types
of information about swallowing but do not results in pictures
of the swallowing process or the food being swallowed. Instead,
most result in amplitude over time displays of the swallow
parameters being examined.
Electromyography: EMG of muscles involved in swallowing
can provide information on the timing and relative amplitude
of selected muscles contraction during swallowing. The
electromyogram is recommended to ascertain the presence
of specific nerve or neuromuscular unit deficit such as that
accompanying vocal fold paralysis or to elucidate or corroborate
the presence of systemic myopathy or degenerative disorders.
The goals of a laryngeal EMG are to detect normal from
abnormal activity and localize and assess the severity of a
focal leision by determining whether there is neuroaphraxia
(physiological nerve block or focal injury with intact nerve fibers
or axonotmesis) damage to nerve fibers leading to complete
peripheral degeneration. Laryngeal EMG can evaluate prognosis
too.
The thyroarytenoid muscle is approached by insertion of
a monopolar or concentric electrode through the cricothyroid
ligament midline 0.5cm to 1.0cm then angled superiorly 45 °C and
laterally 20 °C for a total depth of 2cm. The cricothyroid muscle
is reached by inserting the electrode 0.5cm off the midline, then
angling superiorly and laterally 20 degrees towards the inferior
border of thyroid cartilage. Laryngeal EMG help differentiating
neurological vocal cord paralysis from laryngeal joint injury. It
may also confirm the diagnosis of joint dislocation. The 3 areas
of interest for electro diagnostic evaluation of swallowing are the
laryngeal sphincter, the sensory ability of the supraglottic larynx
and pharynx (indirectly evaluated through cricothyroid muscle
function) and the cricopharyngeal sphincter. EMG has several
pitfalls like precise site of lesion cannot be determined except
whether it involves vagus nerve (SLN and RLN). PCA is difficult
to localize through this. Systemic neuromuscular diseases cannot
be differentiated from focal lesions.
Direct laryngoscopy: Endoscopy of the upper aerodigestive
tract is recommended to rule out biopsy or neoplasm that may
be suspected to be the cause of dysphagia or odynophagia.
Occasionally, the endoscopy may be part of the treatment as
in those patients requiring injection of the paralyzed vocal
fold, injection of BOTOX or dilation of the oesophagus for the
treatment of cricopharyngeal achalasia or strictures.
Electroglottography: EGG is designed to track vocal fold
movement by recording the impedance changes as the vocal
folds move toward away from each other during phonation. This
equipment can be modified to track laryngeal elevation which
can be useful in determining the onset and termination of a
pharyngeal swallow and in providing biofeedback to an extent
and duration of laryngeal elevation during the swallows in which
the patient is attempting to improve these swallow parameters.
Esophagoscopy/Gastroscopy: Dysphagia and odynophagia
are common indications for upper Gastro intestinal endoscopy
and may be performed as the initial test in the evaluation of these
disorders. The esophagus is intubated under direct visualization
of hypopharynx. The endoscope is usually advanced through the
upper esophageal sphincter which appears as a slit like opening
in the cricopharyngeous muscle at about 20 cm from the incisor
teeth. The entire length of the esophagus is indirect view of the
endoscope until its termination at the gastroesophageal junction
which lies at the diaphragmatic hiatus.
The esophagus is usually closed at gastroesophageal junction
but this is easily distended with air insufflations. This allows
the endoscope to easily advance through the lower esophageal
sphincter into the stomach. Upper GI flexible endoscopy is the
most specific test for identifying esophageal complications of
GERD, esophageal ulcer, infectious disorders and neoplasms. It
is useful in defining the cause of disease in those patients with
solid food dysphagia.
Cervical Auscultation (Listening to and recording the
sounds of swallowing): Recording the sounds produced during
the swallow by placing a small microphone or accelerometer
on the surface of the patients neck at various locations has
identified some repeatable sounds produced across normal
subjects (Hamlet, Nelson & Patterson, 1990; Patterson, Hamlet,
Fleming & Zones, 1992). Another method for listening to the
sounds of swallowing is to apply a stethoscope to the patients
neck. The ability to distinguish normal from abnormal sounds or
a define the meaning of the sounds produced during swallow by
patients with swallowing disorders has not been determined. It
needs further research.
Cervical auscultation (Sounds of respiration): This can
define inhalatory and expiratory phases of the respiratory cycle
as well as the moment when the pharyngeal swallow occurs
and in which part of the respiratory cycle, swallowing occurs.
If the secretions are in the airway before or after the swallow,
these will also be heard, as will any changes in secretion levels before and after the swallow. Information on secretion levels
and changes in these levels before and after the swallow may be
indicators of aspiration.
Esophageal Ph monitoring: Prolonged (24hour) esophageal
pH monitoring is the most reliable test for diagnosing GERD.
Twenty four hour pH monitoring is usually done following an
overnight fast. The pH catheter is inserted trans-nasally into
the esophagus. Standard placement of the distal probe is at a
position that is approximately 5cm above the proximal border
of the lower esophageal sphincter. It is ultimately attached to
recording device. Patients are asked to record in a diary or in
the recording device, the times that they eat, sleep or perform
any other activities. More importantly, patients will be asked to
record any type of discomfort that they have including all the
symptoms they experience. This information will be used to
correlate the pH at the time a symptom or activity took place and
a symptom index can be calculated. pH should be less than 4 in
normal individuals.
Manometry
- Esophageal manometry.
- Pharyngeal manometry.
Pharyngeal manometry: The response of the oropharynx
to swallowing has two components. The first is compression of
the catheter against the pharyngeal wall by the tongue which
results in a high sharp peaked amplitude pressure wave. This is
followed by low amplitude, long duration wave, which reflects
the initiation of pharyngeal peristalsis. A rapid, high amplitude
pressure upstroke ending in a single sharp peak, followed by a
rapid return to baseline is produced by contraction of middle
and inferior pharyngeal constrictor muscles to provide mid
pharyngeal response to swallowing.
The pharynx is not radially symmetrical and therefore, the
measurements obtained during standard manometry vary with
the catheter placement. Nonetheless, measurements of intrabolus
pressures during the pharyngeal phase of swallowing may
predict which patients will respond to a surgical myotomy. A
polyvinyl catheter, a thin tube about 35 cm long made of a flexible
polyvinyl material and constructed with multiple pressure
sensors, is passed trans-nasally and the patient is instructed
to perform a series of wet and dry swallows. Lower esophageal
sphincter pressure is measured at baseline and in response to
a swallow. Lower esophageal sphincter pressure is measured
as a step up in pressure from gastric baseline referenced as
atmospheric.
Complete lower esophageal sphincter relaxation with
swallow is demonstrated by a decrease in pressure to gastric
baseline for approximately 6 seconds. Basal, upper esophageal
sphincter pressures can be identified as a rise in pressure above
the esophageal baseline. Due to the asymmetry of the upper
esophageal sphincter, this is normally 50 – 100mm Hg depending
on duration of the pressure sensor (whether lateral or anterior/
posterior). Evaluation of upper esophageal sphincter relaxation
and correlation of sphincter relaxation with pharyngeal
contraction is obtained by instructing the patient to perform a
series of wet swallows.
Acoustical analysis: This is more accessible for speech
language pathologist- done or useful in individuals with mild
dyphagia. Here we will be measuring the swallow sound and
comparing it with the normative developed
Mechanism of the production of glottal sound: It is known
that arytenoids closure, true vocal folds and laryngeal elevation
provide the basis for laryngeal closure during swallowing. The
mechanism of arytenoids closure and true vocal cord closure
valves the larynx shut. In valving the airway during the period
of deglutition apnea, the sub-glottal sound is pressurized. When
the cords apart, there is a release of air and there is a rapid
increase in airflow and the release of this is often audible. Shaker
et al 1990 show that the simple closure at the level of larynx
may not be sufficient to cause the glottal release sound. They say
sudden removal of the valve coupled with elastic recoil of the
lungs provides us with the environment required to produce the
glottal release sound.
Recording of the glottal release sound: Subjects should
be seated in a back straight chair. The cervical region should be
cleansed with a alcohol swipe. The microphone should secured to
the cervical region at the midline of the cricoid cartilage using a
single sided surgical tape such that there is no air escape around
the microphone. Then it should be attached to the preamplifier
which will feed the acoustical signal directly to the computerized speech science lab (CSL 4300, Kay Elemetrics) or any software
which has spectrographic analysis.
Subject should be given trials of water swallow to allow the
investigator to set the optimal recording level. Subjects should
be requested to swallow in one complete action. Recording of the
swallow sound commenced upon the lip cup contact. Recording
ceased post swallow after the laryngeal movement has been
visualized and the individual brought the cup back to the rest
position. Recording should be done directly on to the disk. Each
swallow should be displayed as a raw acoustic signal and linked
by curser and its narrow band spectrogram. The beginning of
swallow sound was marked by combination of auditory feedback
and visual inspection of the spectrogram. Parameters which
need to be measured include frequency, intensity and duration.
This needs to be compared with norms of particular age with
varying thicknesses of fluid as shown in the Table 1 & Figure 1.
Nutritional concerns and assessment in dysphagia
Successful management of dietary needs in dysphagic
patients requires the efforts of all involved caregivers. The
particular responsibility of the dietitian is to assess a patient’s
nutrition and hydration needs and to translate these needs into a
diet that meets restrictions imposed by the team, i.e., oral feeding,
oral feeding with compensatory safeguards or facilitators, enteral
feeding, or combined enternal and oral feeding. As these needs
change, the dietitian should be involved to make the transition
as effective as possible. Another important responsibility of
the dietitian is to make the diet prescribed as appealing and
palatable to a patient as possible.
Both screening and comprehensive nutritional evaluations
require consideration of a patient’s anthropometric
characteristics, dietary intake, relevant clinical and physical
findings and socioeconomic considerations. Comprehensive
assessment will elaborate each of these areas, for example,
dietary intake will be assessed in terms of calories, protein,vitamins, minerals and fluid and evaluated for adequacy based
on the patient’s individual needs.
Indications Nutritional assessment should be considered
when a patient’s mean of feeding has been altered, when such
a change is anticipated, or when there are concerns about the
amount and / or nutrition/hydration value of a patient’s diet.
Populations considered here are those most likely to benefit
from a team evaluation, for example, patients for whom there
are a possibility of safe oral feeding and whose mentation level
is judged adequate for at least a minimal level of cooperation
with team objective. Age groupings of patients have additional
significance. For example, one can expect the CVA (cerebral
vascular accident) population to be older, in general, and the head
trauma population to be younger. Such differences not only have
implications for dietary needs, but also may influence a patient’s
eligibility for funding sources, which support nutritional needs.
In some populations, a change in eating status is anticipated,
and dietary needs can be addressed prior to the expected event.
In other populations, the need for nutritional assistance is acute
and unanticipated. Patients who are apparently well and then
experience a sudden insult, i.e., CVA or trauma are examples of this
kind of population. Other patients may be maintaining adequate
nutrition / hydration but have few reserves to cope with new
or unexpected problems that compromise their nutritional well
being. In such cases, changes in nutrition / hydration status are
not entirely unanticipated. Careful monitoring to assure prompt
intervention is necessary.
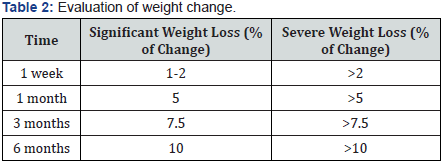
Red flags’ for formal dietitian consult: Significant changes
in weight trends and hydration status in a patient signal the
need for a comprehensive nutritional evaluation. Guidelines
for determining the severity of unintentional weight loss are
presented in Table 2. In general, a person losing 10-20% of his
or her usual weight may sustain moderate impairment, whereas
a loss of greater than 20% of usual weight indicates severe
impairment. In both situations, thorough elaboration of the
cause of weight loss will be required.
Red flags for sub optimal hydration include rapid weight loss
(a 48 hour weight loss of 4 pounds can mean a negative fluid
balance of 2 liters), complaint of thirst, skin turgor changes,
decreased urination, a rising blood-urea-nitrogen level (BUN)
in the absence of other renal indicators, and an increased
serum sodium level (hypernatremia). Patients with thin liquid
dysphagia may be at particular risk for alterations in hydration
status. They will have difficulty augmenting fluid intake to compensate or increased fluid losses due to secondary illness
and are also more vulnerable to other fluid-depleting conditions
(i.e., fever, diarrhea, or increased perspiration related to physical
exertion or heat).
Nutritional assessment: As noted, careful monitoring of
patient’s nutritional status can and should be undertaken by
members of dysphagia team and other caregivers. However,
expedient referral to the dietitian is indicated when there is any
question regarding the patient’s ability to maintain adequate
nutrition / hydration, safely, via the current mean of food intake.
Components of the dietitian’s examination include the following.
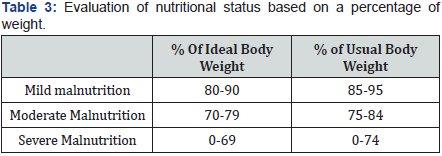
Anthropometric data: As indicated, a primary cue for
dietary referral is weight change. Appropriate weight range is
impacted by gender, age, height and frame. The patient’s usual
weight any change in this amount, over what period of time,
and whether any change was intentional must be determined.
If weight loss is too rapid, and in particular if it is associated
with inadequate protein intake, it may adversely impact the
body’s immune function. The ability to resist disease and
infection is compromised. The patient’s energy level and ability
to participate in the prescribed rehabilitation program may also
be affected. Presented in Table 3 are guidelines for interpreting
nutritional status based on percent of ideal body weight (IBW)
and percent of usual body weight (UBW).
A value of less than 3.5 to 3.2 is suggestive of the patient being
nutritional risk. Other laboratory tests provide a more sensitive
indicator of current protein status but these may require special
ordering procedures. Laboratory values that are both commonly
available and useful for evaluating hydration status are serum
sodium and blood urea nitrogen. Elevated values are typical in
the dehydrated patient. Additionally, albumin will be elevated in
dehydration. One needs to remain mindful that hypo albuminia
may be masked by mild to moderate dehydration, resulting
in a falsely normal appearing albumin value due to hemo
concentration. In dehydration, low urine output will occur as the
body seeks to conserve fluid.
Nutrition history: The patient or caregiver is instructed
to record the time food or drink is consumed, the amount
consumed, and a description of the food and how it was prepared,
i.e., steamed, fried, broiled. The amount of food should be
described using standardized measurements. The patient is also
asked to note if this is a typical meal pattern and, if not, what is
different. Any nutrient label information concerning calories and
protein per serving size should also be included in the report. It
is important to appreciate that merely recording one’s dietary
intake may alter the usual pattern of intake.
Additional measures obtained by the dietitian are a recent
(last 24 hours) food intake record is recalled by the patient
(referred to as a ’24-hour recall’) and a food frequency list, which
describes how often the patient has had different types of foods
over a recent time period. From all measures considered, the
dietitian will compare the patient’s dietary intake to standard
referents of dietary requirements. For example, the USDA
Food Guide Pyramid recommendations for daily dietary
requirements include:
- 6-11 servings from the Bread, Cereal, Rice and Pasta Group (provides the dietary base)
- 2-4 servings from the Fruit Group
- 3-5 servings from the Vegetable Group
- 2-3 servings from the Milk, Yogurt and Cheese Group
- 2-3 servings from the Meat, Poultry, Fish, Dry Beans, Eggs, and Nuts Group.
Subsequent monitoring of weight, laboratory values, and the
patient’s global sense of well being will assist in fine tuning the
nutrition goals.
Clinical and physical findings: It is important to stress
that oral cavity structures and their functional integrity impact
both how and what type of nutrition a patient may be able to
manage. For example, the ability to chew to a ground or puree
texture will determine the texture(s) of food that can be offered
to the patient. Also important to the nutritional evaluation is the
patient’s level of physical activity. If activity is very sedentary,
the patient’s energy need and number of calories required will
be low, necessitating the selection of nutrient dense food. This is
to ensure nutritional adequacy of protein, vitamins and minerals
without excess weight gain that would further impact mobility.
Concurrent chronic conditions, such as diabetes, coronary
artery disease, renal and pulmonary impairment that may have
pre-existing diet management in place, must also be noted. A
cardiac patient’s low diet may be inappropriate if the patient is
unable to consume adequate calories while adhering to the low
fat regimen. The initial priority is to maintain weight. Once this
is achieved, a patient may begin incorporating lower fat food
choices if the low fat diet is still desirable. Diabetic diets have
undergone significant changes since 1994. The emphasis is on
individualizing the diet based on the medical nutrition needs.
Alterations in cognitive skills, ability to attend, or to speak
will of course affect communication and social interaction and
have implications for a patient’s compliance with treatment
objectives. Such changes may also trigger depression or a
diminished sense of well being, with resultant decreased appetite
and failure to maintain weight.
Pediatric feeding assessment: Pediatric feeding problems
have been recognized in the literature for the past 30 years.
Although no comprehensive definition of pediatric feeding
problems has been widely accepted, infants and children experiencing feeding difficulties demonstrate either a refusal to
eat orally and / or are unable to sustain oral feedings to maintain
adequate caloric intake. Numerous articles have identified
groups of children who are at risk for feeding problems. See table
for etiologies commonly associated with feeding problems.
Common etiologies associated with feeding problems- Neurological dysfunction.
- Gastrointestinal disease/dysfunction.
- Cardio-respiratory compromise.
- Sensory deprivation.
- Structural anomalies.
- Social-behavioral maladaptation.
A feeding assessment is a comprehensive, systematic
biopsychosocial approach to the evaluation of a child who has
feeding difficulties. The assessment can help professionals
identify potential or actual feeding problems and develop
appropriate interventions.
Pediatric Feeding Assessment- The feeding assessment consists of five parts:
- Case history (obtained prior to evaluating child)
- Nutritional screening, Feeding history, Developmental milestones (obtained from parent or caregiver’s interview)
- Physical Assessment
- Oral reflexes and feeding skills assessment
- Psychosocial international assessment.
Case History
Done before the evaluation of the child. It includes a review
of the infant or child’s:
- Medical history.
- Growth chart.
- Current clinical nutritional status.
Medical history
The medical history review includes evaluating the
perinatal and neonatal history, medical diagnosis, previous
hospitalizations, and significant illnesses. The perinatal and
neonatal history may provide information detailing any fetal
distress, the infant’s response during delivery, prematurity, any
significant congenital anomalies, and any major illness during
the first month of life. Congenital anomalies, central nervous
system insults, or chronic illnesses may affect the child’s ability
to eat orally. Previous hospitalizations and significant illness
can influence the child’s developmental skills including feeding
skills. Child’s refusal to eat, oral motor organization, and / or
ability to sustain adequate oral intake.
Growth chart: It is critical to
review to growth chart to
determine the child’s nutritional status. Prolonged inadequate caloric
intake results in an infant or child nutritionally failing to
thrive. A child is defined as having failure to thrive when:
- The weight for length ratio is <5%
- The weight is <5% or
- The weight percentage has decreased two standard deviations or more.
Other growth charts for some specific patient populations,
such as Down’s syndrome and premature infants, are available.
Current clinical nutritional status: A review of the current
clinical nutritional status should include laboratory tests and
anthropometrics. Laboratory tests can help define nutritional
deficiencies. The most readily available screening tests are
the complete blood count and a chemistry panel. Protein
deficiency (i.e., a low albumin and total protein). Anthropometric
assessment measures triceps, skin fold thickness and mid arm
circumference as a serial indicator of body fat and muscle mass.
Anthropometrics may be a preferred measurement of nutritional
status compared to growth charts when the infant or child’s age
is unclear.
Nutritional screening, feeding history and development
milestones: This information should be elicited from the parent
or caregivers. The feeding history needs to include the parent’s
perception of the feeding problem or difficulty and a thorough
description of the child’s mealtimes. The history should include
type of food, amounts, textures, duration of feeding, physical
environment, and family members usually present, the child’s
behavior, and any interventions tried. A 24-hour dietary recall
of the child’s feeding routine is helpful to assess individual
nutritional patterns.
Physical assessment
An assessment of the child’s general physical appearance and
findings will provide information about the child’s nutritional
status. When performing this assessment, one must consider the
infant or children;
- Behavior.
- Development.
- Physical appearance.
Behavior: When observing the behavioral state, observe
how the child acts. Is the child alert, active, irritable or apathetic?
The alert and rested child provides the most realistic information
about feeding behaviors. Irritability and apathy are commonly
seen with malnutrition.
Development: The developmental assessment involves
observing the child’s fine and gross motor skills and muscle tone.
Is the child performing tasks at the expected age, or is the child
showing some developmental delays? Most children who are
developmentally delayed exhibit some alteration in muscle tone,
either hypertonia or hypotonia. Both the child’s motor skills and
muscle tone influence his or her ability to eat.
Physical appearance: The physical appearance involves
assessing the child’s:
- Skin.
- Hair.
- Eyes.
- Mouth and oral cavity.
Skin: First, check the skin for color, bruises, rashes, and
turgor. A pale color may indicate iron-deficiency anemia.
Bruising may be due to vitamin K deficiency. Essential fatty
acids, zinc or vitamin deficiencies are known to cause skin
rashes. When inadequate fluid intake accompanies poor caloric
intake, the skin will be dry. Loose skin covering the decreased
subcutaneous fat indicates both a calorie and protein inadequacy
(marasmus). Excessive fluid retention resulting in edema may be
due to insufficient protein intake (kwashiorkor) or electrolyte
imbalances.
Hair: Check hair for texture, color and distribution. Hair that
is brittle, pale blond colored and sparsely distributed is seen
with protein malnutrition.
Eyes: Check eyes for hydration status and infection.
Xerophthalmia, or dryness, may be due to vitamin A deficiency.
Malnutrition can affect the immune system and cause
conjunctivitis.
Mouthand oral cavity: The physical appearance of the
mouth and oral cavity portion are checked as part of the oral
reflexes and feeding skills evaluation.
Psychosocial feeding assessment: The relationship
and interaction between parents and infant or caregiver are
important. This interaction may have profound effects on the
child’s nutrition and feeding. For ex, the parents may be confused
and not offer food to their infant if the infant does not provide
clear hunger cues (ie, agitation, crying and mouth opening).
In cobtrast, the infant who does provide clear cues may not be
offered food coz parents are insensitive to those cues. Therefore
the quality of interaction between parents and their infants have
a very significant impact on the amount of food ingested even if
the infant has normal feeding skills. An interaction assessment
tool such as Nursing Child Assessment Feeding Scale (NCFAS).This provides information about the relationship between the
child and parents.
Oral reflexes and feeding skills: The infant or child’s
reflexes and feeding skills determine the types of foods safely
handled. During the first 3 years of life, dramatic oral motor
and developmental feeding skill changes have profound effects
on the types of food, textures, and feeding methods and the
infant/child can safely control. The approach recommended for
assessing oral reflexes and feeding skills is to progress from the
least frightening or threatening (external touching of the face
and mouth) to the most threatening (internal inspection of the
mouth).
Some oral reflexes are common to all ages, but the most rapid
oral reflex are feeding skills changes occur in infancy. Therefore,
the oral reflexes and feeding skills assessments will be divided
into eight infant developmental stages covering the 3 years of
life.
To know more about Journal of Head Neck please
click on :
To know more about Open access Journals
Publishers please click on : Juniper Publishers

Comments
Post a Comment