Fusion Rates with Autologous Bone Grafts in Pediatric Patients Undergoing Posterior Cervical Spine Fusion
Journal of Head Neck & Spine Surgery Juniper Publishers

Abstract
Objective: Surgical management of cervical instability and obtaining solid bone fusion in children is technically challenging due to smaller and immature anatomy besides the lack of pediatric-adapted instrumentation. Optimizing fusion via additional bone grafting and postoperative HALO device application has been a topic of controversy. We describe our experience with posterior cervical spine fusion techniques and re-visit the role of autologous bone grafting.
Methods: We performed a retrospective chart review of children, who underwent rigid instrumentation and/or onlay bone graft fusion between 2008 and 2019. The primary outcome was solid bone fusion at 2 years after surgery. Secondary outcomes were neurological outcome and adverse events, including surgical and postoperative complications, graded according to the Spinal Adverse Events Severity System, version 2 (SAVES-V2).
Results: Twenty-one patients had a minimum follow up of 2 years (mean 4.65 years, range: 2.0 – 10.68 years), including 14 males and 7 females. The mean age at surgery was 8.4 years (median 8, range 0.7 – 14 years). Indications for surgical fusion were C1/2 instability, secondary instability after surgery, trauma and other etiologies. Seventeen patients underwent rigid instrumentation with application of autologous bone graft and 4 patients onlay bone graft fusion only. Thirteen patients underwent postoperative HALO vest application. Final solid bone fusion was achieved in 19 patients, including 2 with asymptomatic hardware failure. Nonunion and worsening junctional kyphosis required revision surgery in 2 patients. Neurological status remained unchanged postoperatively and at last follow-up. The surgical complication rate was 14%, the overall complication rate 23% respectively.
Conclusion: Variable fusion techniques of the cervical spine can be safely performed and result in adequate fixation in children. Autologous bone grafting is substantially contributing to solid fusion while having a low morbidity profile.
Keywords: Posterior cervical spine instrumentation; Pediatric; Fusion; Bone graft; Autologous
Abbreviations: BMP: Bone Morphogenetic Proteins; CT: Computer Tomography; FU: Follow Up; MEPs: Motor Evoked Potentials; MRI: Magnet Resonance Imaging; PSIF: Posterior Spinal Instrumented Fusion; SSEPs: Somatosensory Evoked Potentials
Introduction
The quality of bone fusion is one of the most critical outcomes in the surgical management of cervical instability. It highly contributes to the rate of revision surgeries and overall long-term outcome [1,2]. Especially in children the surgical management of cervical instability and achieving solid fusion is technically challenging due to the age-dependent variation of anatomy and the lack of pediatric-adapted instrumentation hardware and tools [3,4].
Importantly, the different subset of etiologies resulting in instability of the pediatric cervical spine comprise acquired, but also congenital, syndromic and developmental disorders, which differ from adult pathologies which are characterized by mostly degenerative and traumatic origins. Accordingly, surgical techniques transferred from adults to pediatrics required technical adjustments and flexibility in their application [4]. Given the growing and immature nature of the pediatric spine additional amendments are necessary in order to anticipate the variable anatomy and secondary adverse effects such as adjacent segment degeneration and reduced future growth, depending on the levels and length of the construct [5,6]. Different instrumentation techniques of the pediatric cervical spine have been described, including non-rigid techniques such as external fixation (HALOvest immobilization), variable techniques of internal fixation and onlay bone grafting only [2,7-9].
Supplemental measures of enhancing fusion include the postoperative application of an external HALO device as well as autologous bone grafting or the application of bone morphogenic protein combined with cancellous morselized allograft during the surgery [10]. Despite their assumed benefit of optimizing postoperative fusion, both of these techniques remain subject of a controversial discussion in previous outcome reports with respect to invasiveness, associated morbidity for autologous bone grafting, compliance and necessity for the external HALO device, respectively [11-15]. We describe our experience with posterior cervical spine fusion techniques in children and re-visit the role of autologous bone grafting.
Clinical Material and Methods
We performed a single center, retrospective observational study including pediatric patients with diagnosed cervical instability, who underwent a first time posterior cervical spinal instrumentation, combined anterior and posterior instrumentation and/or onlay bone graft fusion between January 1, 2008, and December 31, 2019, at the Hospital for Sick Children Toronto, Canada. Demographic, radiological, and clinical data were gathered through a retrospective chart review according to the following inclusion criteria:
a) Age <18 years at time point of surgery
b) Cervical instability (x-ray, MRI, w/wo neurological deficit).
c) Posterior spinal instrumented fusion (PSIF) or onlay bone graft fusion.
d) Follow-up (FU) >2 years
Exclusion criteria were a follow-up period of less than 2 years as well as incomplete clinical and radiographic follow-up. Clinical characteristics, indications for fusion, neurological examination findings, and the use of external Halo traction or vest pre- and postoperatively were reviewed. The primary outcome was defined as presence of a solid bone fusion at 2 years after surgery on plain and dynamic x-ray films, whereas the secondary outcomes included type and number of revision surgeries, surgical complications and neurological outcome. The radiographic indices for a solid fusion were:
a) Presence of a solid fusion mass on x-ray posterior to the fused segments.
b) Absence of motion in dynamic x-rays.
c) Absence of signs for hardware failure (breakage, dislocation).
d) Absence of halo-sign as indicator for screw loosening.
Approval for the study was obtained from the University of Toronto Research Ethics Board and the study was conducted in accordance with ethics guidelines.
Results
Twenty-one out of 31 patients met the inclusion criteria and had a minimum follow up of 2 years (mean 4.65 years, range: 2.0- 10.68 years). The remaining 10 patients had not completed the 2-year follow up at the time point of study submission. The sex distribution was 2:1, with 14 males and 7 females. The mean age at surgery was 8.4 years (median 8 years, range 0.7-14 years). Indications for surgical fusion were C1/2 instability (9 patients), secondary instability after tumor surgery (5 patients), trauma (2 patients) and other etiologies (5 patients). Importantly, most of the treated cervical instabilities occurred in a syndromic context (8 patients) and congenital disorders (2 patients), 48% respectively. A detailed list of the patients’ demographic data, their fusion levels and their pathologies are given in (Table 1).
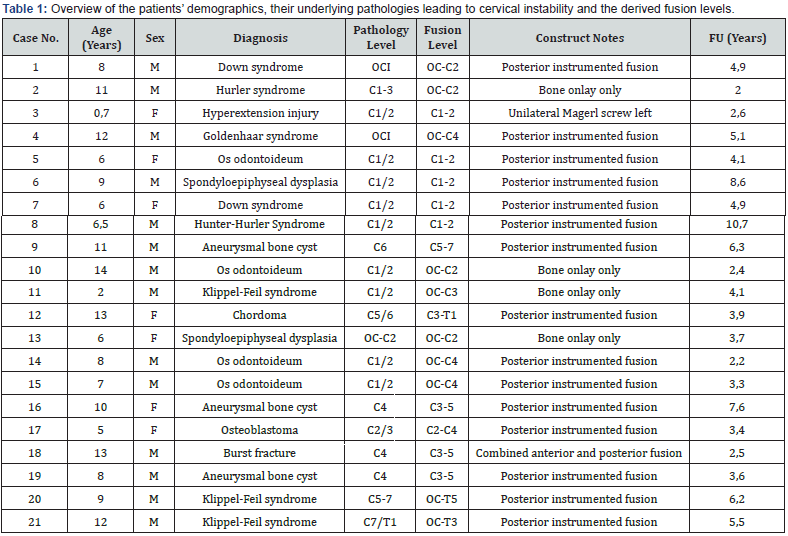
Treatment overview
The diagnosis of cervical instability was determined by assessing a combination of plain and dynamic x-ray studies and magnetic resonance images demonstrating significantly increased mobility in one or more of the three planes of movement (flexion– extension, axial rotation, and lateral bending. Thin-cut computer tomography (CT) scans with 2D sagittal and coronal as well as 3D reconstructions were obtained pre-operatively for surgical planning with respect to the optimal fusion and instrumentation technique. Four patients underwent preoperative HALO traction in order to obtain a closed reduction in the context of subluxation or cervicothoracic dissociation.
Two of them underwent additional HALO vest application as well as 2 other patients with Down syndrome for primary preoperative stabilization. Sixteen patients were submitted to rigid posterior instrumentation and one patient combined anterior and posterior instrumentation, all with intraoperative application of autologous bone graft. We performed an onlay bone graft fusion only in 4 patients. The autologous bone graft was predominantly harvested from the iliac crest (17 patients), followed by the rib (2 patients) and local graft from the spinous processes (2 patients). All of the surgeries were performed with a rigid head fixation in the Mayfield clamp and under neuromonitoring including somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs).
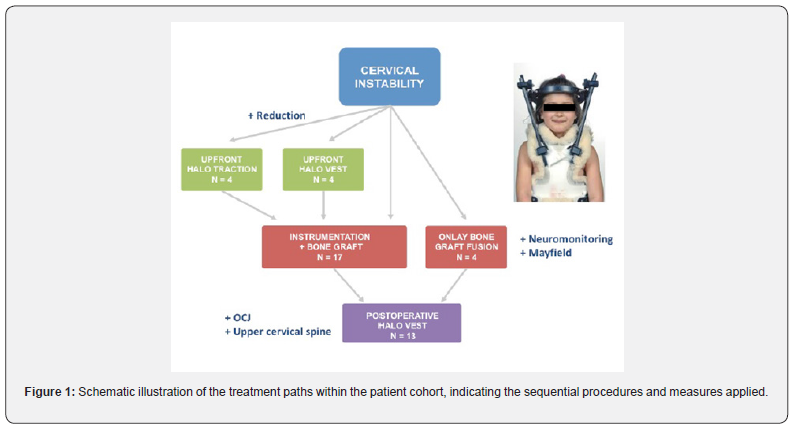
Postoperative HALO vest application was performed in 13 patients, including 8 syndromic patients, 2 patients with a congenital disorder as well as one trauma patient with a severe hyperextension injury. The levels of fusion in all of these patients were located in the upper cervical spine at C1/2 or at the craniocervical junction, including the occiput as upper fixation point. All patients, who underwent posterior cervical fusion with onlay bone graft only were included in this group (Figure 1). The time period for postoperative HALO vest application ranged between 2 and 3 months.
Primary outcome
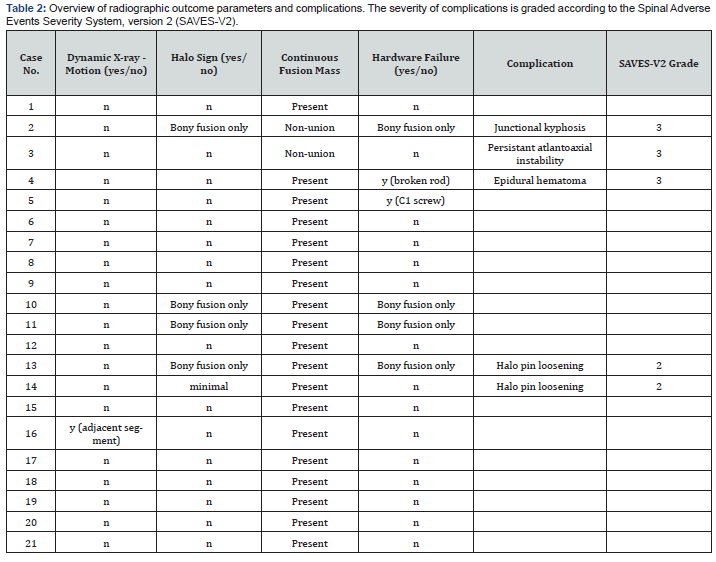
Solid bone fusion was confirmed radiographically via dynamic x-ray and computer tomography in 19 patients (90%) at the 2-year follow-up, including 2 patients with asymptomatic hardware failure. One of them had a rod breakage on one side and the other one a questionable screw loosening, however a solid posterior bone fusion mass was present, and no motion observed in the dynamic x-rays. Nonunion and worsening junctional kyphosis required revision surgery in 2 patients at 5 and 6 months postoperative follow up.
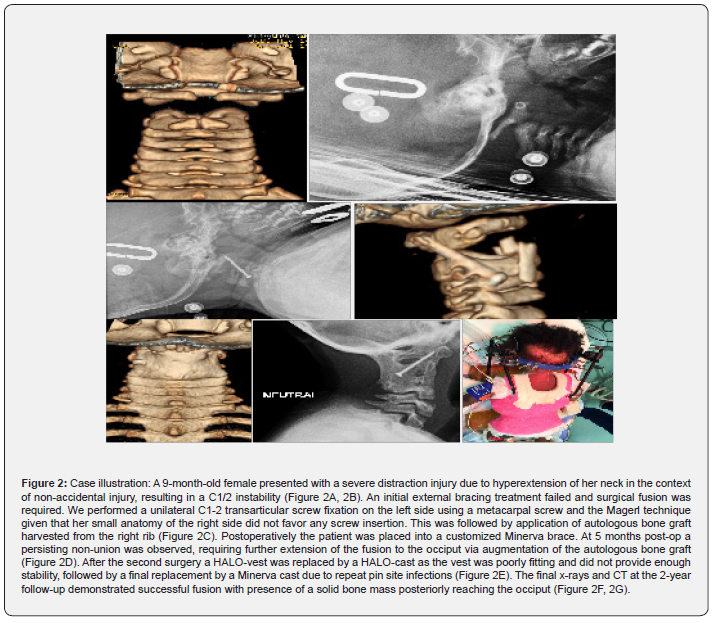
One of these patients with Hurler syndrome had a previous bone onlay only fusion anticipating his small posterior elements, which did not permit primary instrumentation. He required augmentation of the autologous bone with additional grafting from the rib. A nine-month-old female developed a non-union with persistent atlantoaxial instability, equally requiring augmentation of the autologous bone graft and extension of her fusion to C3 (see case illustration, (Figure 2)). The rate of fusion failure in the early postoperative course was 10%. Radiographic data on the fusion outcomes are shown in (Table 2).
Secondary outcomes
The neurological status of all patients remained unchanged postoperatively and at the last follow-up visit. There were no transient neurological deficits observed in the early postoperative course.
Non-fusion related complications were development of an epidural hematoma after HALO ring application in one patient, necessitating emergent surgical decompression. HALO vest adjustments requiring additional sedation occurred in 2 patients. One patient developed repeat pin site infections due to the lack of adequate care and required antibiotic treatment. None of the patients developed a primary surgical site infection or complications related to the bone graft site. The overall complication rate was 23%, including the HALO vest adjustments and complications related to its placement and positioning. Complications and their grading according to the Spinal Adverse Events Severity System, version 2 (SAVES-V2) are indicated in (Table 2) [16].
Discussion
We have described our experience managing cervical instability of various etiologies in 21 children, undergoing surgical fusion with rigid instrumentation or bone onlay grafts only. All patients underwent autologous bone grafting during the index procedure and 90% were confirmed with a solid fusion at the 2-year follow up. Two patients required revision surgery due to non-union and junctional kyphosis, indicating temporary lack of solid fusion. However, solid fusion could be achieved after revision surgery with augmentation of the bone graft in both patients.
Multiple studies reported the use of autologous bone grafting and its impact on obtaining solid fusion [11,12,17,18]. Posterior iliac crest autograft is the preferred substrate for bone graft material, followed by rib graft in youngest children and after multiple fusion attempts. Despite its excellent structural support and its benefit on fusion outcome it remains controversially discussed in regard to morbidity and surgical site complications [2,19]. Several authors discuss a significant morbidity from the autograft harvest site, such as donor site pain, increased blood loss and infection risk, seroma formation, pelvic fracture, and the risk of peripheral nerve injury.
Moreover, it was experienced as a challenge to harvest and craft a well-fitting bone block from a small rib or thin iliac crest in children [1,20,21]. We did not observe any of these morbidities or complications in our cohort. From a technical perspective we equally did not face any challenges in harvesting the bone graft, which might be related to using autograft as a “gold-standard” during deformity surgeries in our institution. Other authors confirmed a clear superiority of autologous bone graft compared to allograft or bone morphogenetic proteins (BMP) and advocate for its continuous use [22,23].
A recent meta-analysis published by Reintjes et al. [20] assessed the fusion rates in 604 pediatric patients undergoing either posterior cervical or occipitocervical instrumented fusion with additional grafting of autologous bone in 539 and in 65 patients with application of allograft. Higher overall fusion rates were observed in the autologous compared to the allograft group (94% vs 80%) [20]. In our study autologous bone graft was applied to 21 patients, of which 2 demonstrated a shortterm postoperative fusion failure (10%) resulting in a fusion rate of 90%. These results are concordant with previous reports and confirm the benefit of autologous bone grafting with a low morbidity profile. Importantly, we could demonstrate overall good fusion results in patients with bone onlay graft only.
The 4 patients were 2, 6, 11 and 14 years old, suggesting that success of this technique is not necessarily restricted to a specific age group or younger children. However, randomized controlled trials are warranted in order to compare the efficiency and outcomes of rigid instrumentation versus onlay bone graft only. Another important point of discussion is the pre- and postoperative use of HALO devices. They were applied in the majority of our patients, 13 patients (62%) respectively. The reasoning was either to achieve preoperative reduction or to facilitate postoperative fusion.
Latter one might be particularly at risk in patients with cerebral palsy, in syndromic and youngest patients, who might present with abnormal movements or compromised compliance. Furthermore, given the softer bone texture there is a higher complication rate related to implant pull-out in these pediatric patients. In this context HALO vest application after posterior cervical fusion has been shown to be beneficial. Moreover, we do think that fusions performed with onlay bone graft only mandate postoperative external stabilization in order to facilitate a solid bone fusion. Despite not having experienced many pin site infections, except in one patient, we confirm a higher complication rate in patients with HALO devices.
These are either related to readjustments, requiring most of the time sedation and complications that occurred during placement of the device per se. Although HALO devices are related to a higher complication profile, they outweighed in our patient cohort with many complex and syndromic patients the risk of implant pull-out and nonunion. Previous studies reported similar complications, but also an increased fusion rate in patients with postoperative HALO vest or Minerva cast application [24,25]. Thus, the indication for HALO devices needs to be adapted to the underlying pathology, degree of instability, levels of fusion and the compliance of the patient, outweighing its risks and benefits in a critical manner.
Limitations of the study are the small number of patients, especially in the onlay bone graft group as well as the confounding factor of not having a control group, undergoing rigid instrumentation without additional application of autologous bone graft.
Conclusion
In this study, we found that the variable fusion techniques of the pediatric cervical spine can be safely performed and represent an effective way to treat cervical instability in various pathologies and patient ages. The supplemental application of autologous bone graft increases the quality of fusion while having a low morbidity profile with respect to the grafting site. The use of postoperative HALO vest application can be advantageous in syndromic patients and those, who undergo fusion of the upper cervical spine and the craniocervical junction in order to enhance the construct stability and fusion onset. Further studies with larger patient numbers are required to confirm these findings.
To Know More About Journal of Head Neck & Spine Surgery Please click on:
For more Open Access Journals in Juniper Publishers please click on:
Comments
Post a Comment