Postsurgical Complications after Spine Surgery-Juniper Publishers
Juniper Publishers-Open Access Journal of Head Neck & Spine Surgery
Postsurgical Complications after Spine Surgery
Abstract
We present a case of a 22-month-old infant who undergoes a surgical procedure consisting of performing cervical arthrodesis after placement of a halo of cervical traction and thoracic harness. The patient presented an alteration in the formation and segmentation of the cervico-dorsal vertebral bodies, alteration of the vertebral canal and angulation of the medullary cord. In the postoperative period, the main complications are intense pain that requires intensification of sedo analgesia, sepsis, diaphragmatic paralysis secondary to surgery, and respiratory and hepatic failure due to chest compression of the harness.
Keywords: Vertebral malformation; Pain Cervical halo; Thoracic harness; Respiratory failure; Liver failure
Abbrevations: ICU: Intensive Care Unit; CT: Computed Tomography
Introduction
The malformations of the spine are a group of polymorphic anomalies, from small asymptomatic lesions to important disorders responsible for vertebral deformities, neurological disorders and even respiratory failure. The orthopedic and neurosurgical treatment depends on the severity of the clinical affectation [1,2].
Case Report
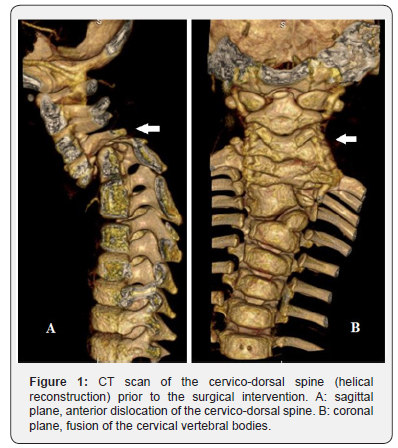
Infant of 22 months with antecedent of alteration in the formation and segmentation of the cervico-dorsal vertebral bodies, alteration of the vertebral canal and angulation of the medullary cord (Figure 1), in follow-up by Rehabilitation and Neurosurgery. She starts at 21 months right brachial palsy, so added to the degree of spinal angulation is indicated neurosurgical intervention consisting of placement of a halo of cervical traction and vertebral arthrodesis in a second time. Enter the pediatric Intensive Care Unit (ICU) after placement of the cervical halo and thoracic harness for adaptation and initial management of pain with sedation. She arrives without invasive ventilation and with spontaneous movements of the four extremities. 24 hours after admission, she presents episodes of desaturation, cyanosis and gasping, with severe respiratory acidosis, which requires orotracheal intubation and connection to invasive mechanical ventilation. Chest x-ray and urgent cranial Computed Tomography (TC) were performed without evidence of postoperative complications. The cervical halo is removed, and the thoracic harness is loosened, presenting frank improvement of ventilation in the following hours. 48 hours after the episode, cervical halo is repositioned, thoracic harness is removed and cervical traction with weight is placed. In the following days, it is necessary to intensify sedo analgesia due to pain. 9 days after admission to the ICU, the surgical intervention was completed by performing vertebral corpectomy with cervical arthrodesis. He returns to the ICU having removed cervical traction with weight, repositioning the thoracic harness and maintaining a cervical halo. Progressive descent of the respiratory support is performed, invasive ventilation being removed 48 hours after the arthrodesis. Subsequently, she tends to hypercapnia and respiratory acidosis. Non-invasive ventilatory support is started, without improvement. Given the suspicion of restrictive etiology due to external thoracic compression, the thoracic harness is loosened, improving thoracic expansion and ventilation. 14 days of admission, she presents hypotension, tachycardia, coagulopathy and fever, which required several volume loads with crystalloids and administration of dopamine in continuous perfusion. Sepsis is suspected, so treatment with meropenem and vancomycin is initiated. In this context, she requires again connect to invasive ventilation due to respiratory failure. 48 hours after the onset of the sepsis, she presents acute liver failure of probable ischemic origin (ALT/LDH ratio <1.5) in the context of hyper transaminasemia (AST 13246 U/L, ALT 5668 U/L), coagulopathy and hepatomegaly. Given the suspicionof mechanical compromise by the harness, it is immediately removed, and the treatment is adjusted by removing the drugs with hepatic metabolism. Treatment of acute liver failure is initiated, adding treatment with carbaglumic acid to hyperammonemia, N-acetylcysteine and liposomal amphotericin B as prophylaxis. She begins progressive improvement of hepatic insufficiency and septic shock by suspending dopamine support 4 days after, allowing a decrease in respiratory support and sedo analgesia. Germs are not isolated in the collected blood cultures. 9 days after the septic shock, cervical halo and invasive mechanical ventilation are removed.
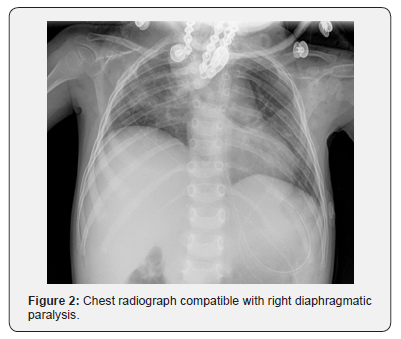
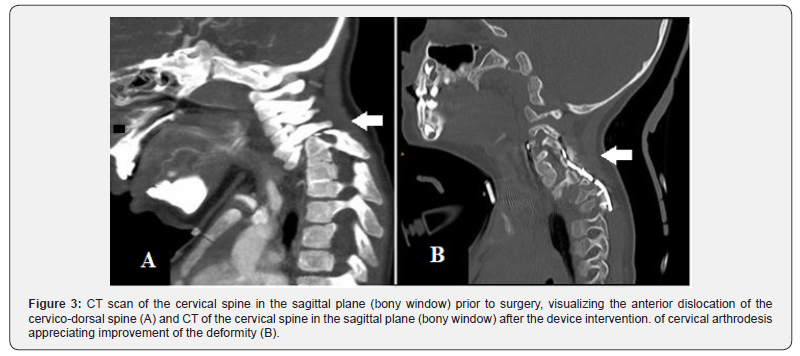
She presents again respiratory failure and right diaphragmatic paralysis secondary to surgery is suspected, which is confirmed by radiological and neurophysiological study (Figure 2). In the following weeks she presents a torpid evolution. She tends to hypertension in the context of withdrawal syndrome and requires an increase in sedo analgesia. In view of the difficulty in permanently removing invasive mechanical ventilation associated with the presence of a justifiable cause of respiratory failure and being a patient with difficult intubation, a tracheostomy was performed. The intermittent disconnection of the respirator begins in the following weeks. It is possible to normalize the blood pressure and resolve the withdrawal syndrome. During the evolution she presents difficulties in the tolerance of the enteral nutrition and in the oral intake, deciding to perform a gastrostomy. CT of the cervical spine performed one month after the intervention shows an improvement in the vertebral malformation (Figure 3).
Discussion
Malformations of the spine require management by a multidisciplinary team. Early diagnosis allows early initiation of rehabilitative and orthopedic treatment in those cases that require it. Depending on the type, they can cause scoliosis and / or developmental congenital kyphosis and surgical treatment is required the first years of life [1]. In this case, the neurosurgical indication is posed after the onset of brachial palsy in addition to the vital risk due to spinal cord angulation. During the postoperative period, the main complications are pain management and withdrawal syndrome, a septic shock, respiratory and liver failure, secondary to chest compression due to the harness and diaphragmatic paralysis secondary to surgery. The episode of severe respiratory acidosis that appears 24 hours after admission is considered due to carbon dioxide intoxication due to hypercapnia secondary to hypoventilation due to the thoracic harness.
The ischemic liver failure is a rare cause of acute liver failure both in childhood and in adults. The etiopathogenesis involves low cardiac output secondary to postoperative cardiovascular surgery, sepsis and extrinsic abdominal compression [3]. In this case, it is believed that low cardiac output is involved due to the septic pattern and the decrease in hepatic blood flow secondary to compression by the thoracic harness. From the histological point of view, ischemic hepatitis is characterized by originating centrilobular necrosis with absence of inflammatory elements [4]. At the analytical level, it is characterized by a marked and reversible elevation of the transaminases and the LDH enzyme with an ALT/LDH ratio lower than 1.5. The treatment of ischemic hepatitis includes the management of the underlying cause and supportive treatment of liver failure. It tends to resolve quickly after the improvement of the underlying cause. However, delay in diagnosis implies worse results [5]. In this case, the transaminases fell quickly, reducing to a quarter after 48 hours of withdrawing the thoracic harness and normalizing after 15 days. Another of the main postoperative complications was diaphragmatic paralysis, which although infrequent, can trigger an important respiratory compromise. It should be suspected especially in the postoperative period of thoracic and cardiac surgery when there is unexplained difficulty todecrease the respiratory assistance or after a failed extubation. The chest radiograph shows a marked elevation of the affected hemidiaphragm. The ultrasound allows a dynamic study of the diaphragm and determines if there is absence or decrease in diaphragmatic mobility. Electromyography allows to evaluate the phrenic nerve and the diaphragm. The treatment can be conservative, based on respiratory rehabilitation, or surgical. There is not consensus as to which is the most appropriate [6,7].
Several of the postsurgical complications presented by the patient were secondary to the use of the thoracic harness. It is a mechanical device used to optimize the traction function of the cervical halo. However, due to the mechanism, it compromises respiratory and circulatory function, especially in pediatric patients. The presented case is considered instructive since there was no experience on the use of this device in children. For this reason, it is essential for future cases to know the complications due to the use of this type of device.
For more articles in Open access Journal of Head Neck & Spine Surgery | please click on: https://juniperpublishers.com/jhnss/index.php
For more about Juniper Publishers | please click on: https://juniperpublishers.com/pdf/Peer-Review-System.pdf

Comments
Post a Comment