Unusual Case of Nasopharyngeal Carcinoma with Intracranial Metastasis without Direct Invasion-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Introduction
Nasopharyngeal Carcinoma (NPC) is a rare malignancy
in Western countries but considered endemic in certain places such as
southern China and Southeast Asia [1] In Malaysia, NPC is the fifth
(4.9%) most common cancer among Malaysians and the third (8.1%) most
common cancer among males [2]. Because of nasopharyngeal anatomical
location, patients with locally advanced NPC, it is not infrequent that
the primary tumor directly invades the intracranial sites such as
cavernous sinus through the skull base. Distant metastases to Central
Nervous System (CNS) either through hematogenous route or Cerebral
Spinal Fluid (CSF) spread are rare and dural metastasis at parietal
region is even extremely rarer [3]. In this article, we report a rare of
an elderly man with left parietal dural metastasis from NPC.
Case Report
A 65-year-old male was diagnosed with T2N1M0-Stage II
NPC (American Joint Committee on Cancer (AJCC, 7 edition)) back in
2015. A Magnetic Resonance Imaging (MRI) scan and fiber optic endoscopy
revealed a small primary tumor in left lateral nasopharynx and the
biopsy revealed undifferentiated carcinoma of the nasopharynx. There was
no intracranial extension but presence of metastatic lymph node
measuring 1.5cm in greatest dimension over right neck. Three cycles of
cisplatin based combined chemotherapy regimen (cisplatin,
5-flourouracil) were given prior to radiotherapy and a complete response
was obtained at both primary site and in the neck. The nasopharynx and
regional lymphatics were treated to a total dose of 34 fractionwith
conventional radiotherapy regimen. He subsequent received a Concurrent
Chemoradiotherapy (CCRT), which was finally completed in May 2017.
Patient had been on surveillance follow up with Oncology team since
then.
He remained well until 2 years after the conclusion
of the radiotherapy, when he presented with pain over the left chest
region for which a Computed Tomography (CT) Thorax was performed at a
private center. On assessment, there was no neurological deficit
elicited during that time. On CT imaging, there was nodular left pleural
thickening with enhancement with metastasis lesions in thoracic
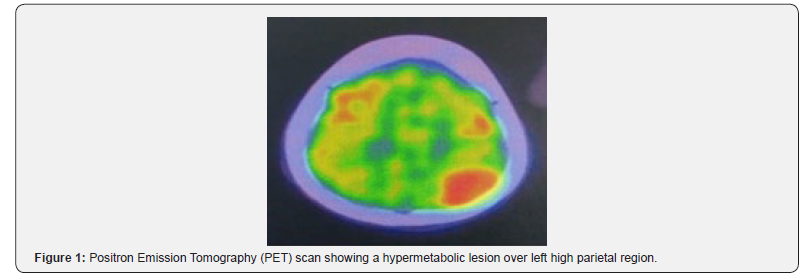
vertebral bodies. Fluorodeoxyglucose positron emission computed
tomography (FDG-PET/CT) scan was done for detailed workup, revealed
pathological uptakes at the left nasopharynx, left pleural, left lung
and a new hypermetabolic hyperdense mass in left higher parietal lobe,
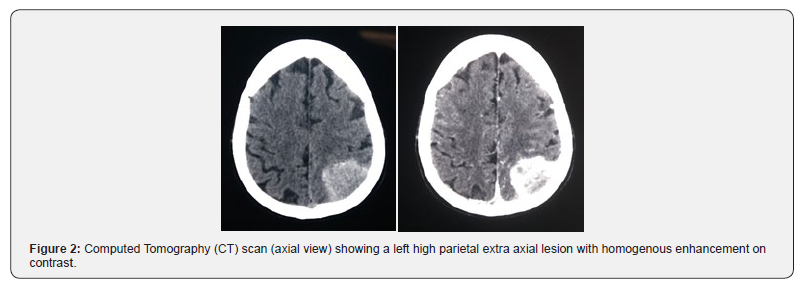
measuring 4.5 x 3.2 cm in size (Figure 1). The extra axial mass enhanced
homogenously at a contrasted enhance CT with minimal edema (Figure 2).
Radiologically unable to rule out possibility of a convexity meningioma
arising from left parietal dura. The brain lesion was excised totally
with a craniotomy and pathological examination revealed metastatic
undifferentiated carcinoma (WHO Grade III).
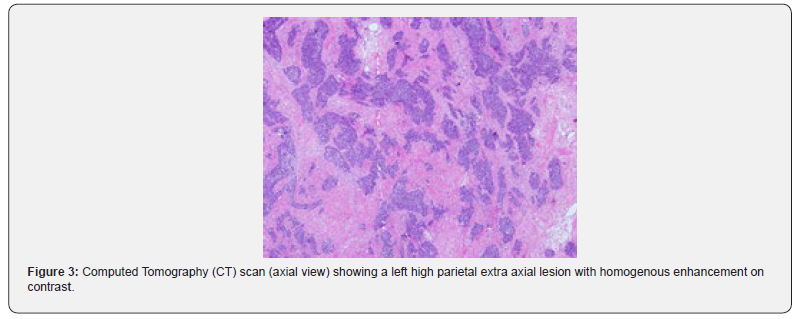
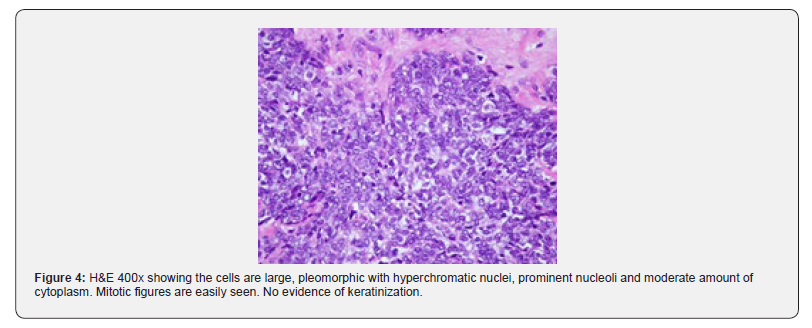
On microscopic examination, the tumor shows fragments
of cellular tissue infiltrated by malignant tumor arranged in syncytial
pattern of cohesive cells with indistinct cell margins. The cells were
large, pleomorphic with hyperchromatic nuclei, prominent nucleoli and
moderate amount of cytoplasm. There was focal necrosis, and high
mitosis. Immunohistochemical study revealedthat the tumor cells showed
membranous CK 5/6 (Cytokeratin
5/6) immunoreactivity (Figure 3&4). Original diagnosis of
the nasopharyngeal mass made in 2015 was confirmed to be
undifferentiated nasopharyngeal carcinoma, which has similar
morphological characteristics as the metastatic carcinoma to the
brain. Post-operative, he was right hemiplegic secondary to infarct
with hemorrhagic transformation. Patient was opted for palliative
care in view next line of chemotherapy is high risk for the patient
with current poor performance status.
Discussion
Even though intracranial invasion by direct extension of locally
advanced disease is not uncommon, metastases to the CNS, either
through hematogenous route or through the Cerebrospinal Fluid
(CSF), from NPC have rarely been reported. Metastatic lesions to
occipital and temporal lobes have been reported in some cases
but for this gentleman, metastatic lesion was located near the
parietal lobe [4, 5]. There is no known lymphatic or vascular
connection between the nasopharynx and parietal lobes. Ngan
and colleagues, discussing the same issue for the patients who
had occipital metastases, hypothesized that microenvironment
in the occipital lobes might have facilitated the metastatic tumor
cells to localize in that region [5]. This case has shown that the
occipital lobe and temporal are not the only sites for NPC cells
to metastasize, thus make this case the first to be reported of a
parietal dural metastasis from NPC. The incidence of recurrence
of NPC has been reported as high as 77.5% following a remission,
in which 48.1% occurs after 2 years while 17.4% recurred after
7-12 months [6]. Concurrent Chemoradiotherapy (CCRT) is the
most potent treatment combination for locoregional control as
well as improve overall survival for the advanced disease [7].
However, the impact of CCRT upon distant control was inadequate
[8]. As for this case even with a good locoregional control post
CCRT, yet after 2 years patient develop new distant metastasis
to lung, vertebral bodies and brain. The 5-year overall survival
rate of non-metastatic locoregionally advanced NPC treated with
radiotherapy is reportedly up to just 60%, while the presence of
distant metastases decreases it further to be around 12-15 months
at best, after chemotherapy [9].
Status of primary tumor, evidences of disseminated
disease,
performance status of the patient, treatment modalities already
applied to the patient, histopathology of the tumor, and symptoms
related to brain metastases are the factors effecting the
therapeuticmanagement. Since there was locoregional recurrence and
patient
was hemiplegic after operation, palliative care was planned for
this patient. Palliative chemotherapy was not given in view his
family members refused. In conclusion, due to the rarity of dural
metastasis from the NPC, a high index of suspicion should be
practiced where 6 monthly or yearly radiological assessments
should be performed to rule out distant metastases including a CT
scan of the brain.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment