Herniotomy Alone as Treatment for Scrotal Migration of Ventriculoperitoneal Shunt-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Complication rate of ventriculoperitoneal (VP) shunt
is from 11%-25%; differs from centre to centre. One of the rare
complications of ventriculoperitoneal shunt is distal catheter migration
into various abdominal contents including the scrotum. A few cases of
scrotal migration of distal catheter have been reported in paediatric
patients with different managements. Here we report a case of a
3-year-old child who presented with a right sided hydrocele with the
distal end of the shunt in the left hemiscrotum 3 years following a VP
shunt placement for congenital hydrocephalus. Herniotomy alone was our
management in this case.
Keywords: Ventriculoperitoneal shunt Scrotal migration Herniotomy
Ventriculoperitoneal (VP) shunts are the most
commonly performed operative procedures to treat hydrocephalus in
children [1]. Shunt migration is one of the rare complications of VP
shunt yet there are a few case reports have reported migration to the
scrotum via patent Processus vaginalis due to the frequent incidence of
shunt placement. In this article we report a rare case; the first out of
180 VPS done in the hospital; who presented with scrotal migration of
VP shunt.
Case History
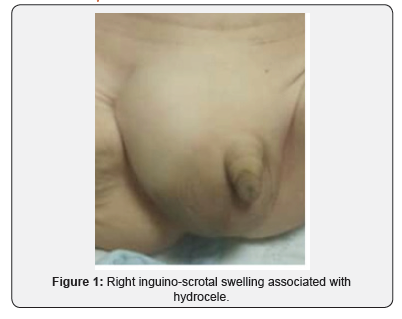
A 3-year-old boy presented with a swelling of the
right inguino-scrotal region since a day prior. He had undergone right
VP shunt procedure for congenital hydrocephalus at the age of 3months.
The swelling was not associated with any complains of
pain, fever or features of intestinal obstruction. On examination
a gross swelling was noted in the right scrotal region (Figure 1).
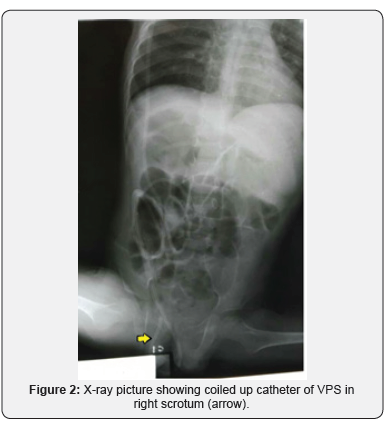
There were no clinical features of shunt malfunction. An X-ray
of the abdomen and pelvis showed that the peritoneal end of
the shunt coiled in the scrotum with its tip inside the abdomen
(Figure 2). Patient asymptomatic of raised ICP and shunt block
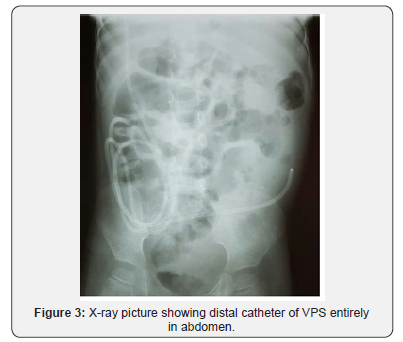
Patient was then planned for herniotomy. Prior incision,
swelling could be reduced under general anaesthesia easily.
Exploration was done subsequent revealed a thicken sac with
empty contents and excised completely. VP shunt catheter was
reduced with hernia sac preoperatively; the catheter was not
visualized intraoperative. Post-operative X-ray confirmed the
replaced entire distal shunt in abdomen (Figure 3). The patient
is currently asymptomatic and doing well at follow-up.
Discussion
VP shunt insertion is a common treatment for hydrocephalus.
The distal catheter of VP shunt can migrate into various body
parts including the ventricle, scalp/subgaleal space, mouth,
neck, breast, breast implant, thoracic cavity, pulmonary artery,
intracardiac, lungs/pleural space/transdiaphragmatic, anterior
chest wall, intraabdominal wall, abdominal subcutaneous fat
tissue, umbilicus, stomach, large intestine, liver, gall bladder,
bladder/urethra, inguinal sac, buttocks, canal of Nuck, which
is the female counterpart of the spermatic cord, vulva/vagina,
rectum/anus, and knee [3]. The reported incidence of distal
migration of VP shunt is 10% [4]. But only less than 40 cases
have been reported on scrotal migration of distal end of the
shunt, as it is a rare phenomenon [5].
Normally, Processes vaginalis is patent at 60-70% of infants
in first three months of life. It could be established as patent
at 50-60% of 1-year olds and 40% for children between ages
2-16 years [6]. Increased abdominal pressure following shunt
insertion may prevent obliteration of the Processus vaginalis
and facilitates migration of the VP shunt into the scrotum [2].
Smaller size of peritoneal cavity in infancy compared with older
children could be another etiologic factor for VP shunt migration
to Processus vaginalis [7].
Scrotal migration of the distal VP shunt can lead to secondary
hydrocoele, incarceration of catheter, and shunt malfunction,
which in turn can cause worsening of the hydrocephalus [5]. A
plain radiographic shunt series should be performed to assess
integrity of VP shunt and plain computed tomography scan is
needed to reassess the severity of hydrocephalus.
Management differs from case to case basis. The most
common management encompassed shunt revision and
herniotomy. Out of 36 cases reported 27 cases was managed with
herniotomy and shunt revision and another 8 cases with shunt
revision with no herniotomy done. Only 1 case was managed via
herniotomy alone alike this case with manual compression of
swollen scrotum [5].
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
Comments
Post a Comment