A Rare Origin of Supraclavicular Mass in a Ten-Month-Old Child: Case Report of Lipoblastoma-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Introduction
Lipoblastoma is a rare benign tumor arising from
embryonic white fat which occurs in the early childhood and accounts for
up to 30% of adipocytic tumors in children while true lipomas account
for 60% of all cases [1]. It usually arises on the extremities and
considered as a rare cause of a pediatric head and neck masses. To
notice that less than 100 cases of lipoblastomas-
all locations- have been reported in literature till now, whereas, head
and neck involvement has been reported in only very few cases [2]. In
the Hospital University Ibn Rochd, we admitted a ten month child with
lipoblastoma arising from the supraclavicular area. A significant risk
of invading the subclavian vessels, the brachial plexus and the thoracic
duct in contact was near.
Case Report
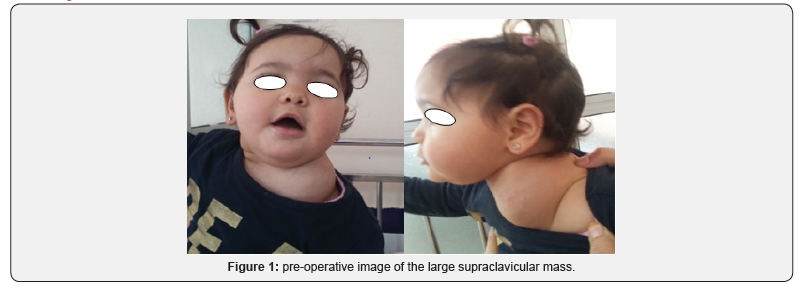
A 10-month-old girl, with no relevant medical or
surgical history, brought by her parents to the outpatient ENT
department for painless left side neck mass growing progressively over
the last 5 months, with no sign of compression, in a context of a
conservation of general state. On physical examination, there was a
painless, non-pulsatile, solid to firm left-sided cervical mass in the
supraclavicular area measuring approximately 6cm of large diameter,
fixed to the underlying structures, mobile relative to the overlying
skin (Figure 1), with no inflammatory signs neither was a lymph node
hypertrophy. The rest of clinical examination was within normal limits
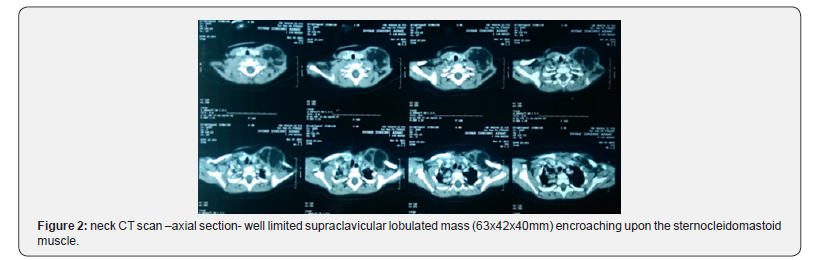
with no abnormal laboratory findings. Ultrasonography revealed a
homogeneous, hyperechogenic mass with a peripheral vascularization,
plunging into the left supraclavicular area evocative of either
hemangioma or lipoblastoma. We completed by neck CT scan which revealed a
well limited supraclavicular lobulated mass encroaching upon the
sternocleidomastoid muscle, with a greasy density similar to that of the
subcutaneous fat in which some enhancement was visible, crossed by
internal septa, measuring 63x42x40mm.The mass came into contact with the
clavicle
without bone lysis, also with the subclavian blood vessels which remain
permeable (Figure 2). The biopsy of the mass confirmed the diagnosis of
lipoblastoma. A multidisciplinary surgery (Otorhinolaryngologist and
Pediatric surgeon) was considered
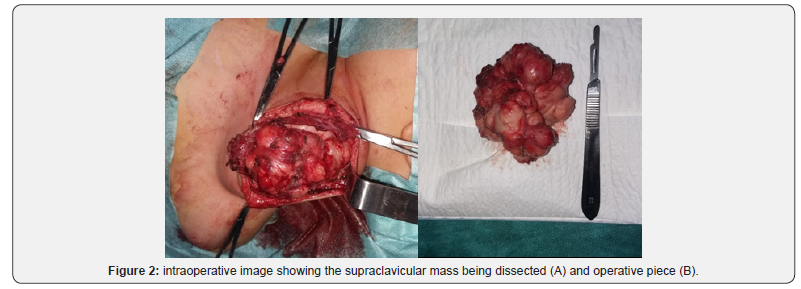
Per-operatively, the lesion was found to be well encapsulated
fixed to clavicle, in contact with the branches of the brachial
plexus posteriorly. Complete surgical resection of the mass
with an under-periosteum dissection without cleidotomy was
performed, the subclavian vein was tightly adherent to the mass
which was delicately dissected, and the brachial plexus was seen
and preserved (Figure 3). Histological examination showed an
adipose lesion, divided into lobules by fibrous septa. The adipose
tissue consisted of mature adipocytes of various size and few
lipoblasts. These findings were compatible with lipoblastoma.
The postoperative period was uneventful, one-year follow-up
found no local recurrence.
Discussion
The term “lipoblastoma” was coined by Jaffe [3] in 1926 to
describe an atypical lipomatous lesion that consisted of cells
resembling embryonic white fat [3]. This term was intended to
differentiate these lesions from common lipomas, which contain
no lipoblasts. Chung & Enzinger [1] described two forms:
lipoblastoma as a localized circumscribed type which represents
approximately 70% of cases and lipoblastomatosis for the diffuse
multicentric variant (about 30% of cases) which is a deeply
located, poorly circumscribed lesion with infiltrative growth
pattern that may affect surrounding muscle structures, this
latter is more difficult to remove completely [1,4]. It commonly
arises from the extremities (36 72%) and the trunk (20 50%),
and less commonly in the head and neck (10 15%) [2]. Within
this latter, the neck is the most common location, other locations
may also be included as the parotid gland, cheek, skin and orbit
[5,6]. It occurs exclusively in infants and children, with 90% of
the cases in children under 3 years of age, with the median age
of onset being 1 year. It shows a male preponderance (3:1) and a
rapid growth rate [6].
Usually, it presents as a painless, progressively growing mass
if localized superficially. Symptoms are related to the location
and size or mass effect of the lesion. Its rapid growth may cause
compressive symptoms such as an airway obstruction and
respiratory symptoms that have been described in patients with
pleural, mediastinal, pulmonary, and lower neck lipoblastomas
[5,7].
The presumptive diagnosis is performed by imaging:
Ultrasonography, CT or MRI being more sensitive by showing the
characteristics of the mass components [7]. Imaging exhibits the
precise location of the lesion and its extent to the surrounding
structures which helps in planning surgical resection, however, it
cannot differentiate lipomatous tumors which make these ones
radiologically indistinguishable [8]. Therefore, the definitive
diagnosis is made histologically. Moreover, recent cytogenetic
analysis revealed specific chromosomal abnormalities in adipose
tissue tumors which may lead to accurate diagnosis [2,9].
The most important differential diagnosis of lipoblastoma
is myxoid liposarcoma. Since the distinction between the twoentities cannot be performed on imaging. The age of the patient
is significant. Liposarcomas are extremely rare in patients less
than 10 years of age. Histology can differentiate on the basis
of architectural changes and cytogenetic analysis displays a
characteristic rearrangement of the long arm of chromosome
8 (8q11-13) affecting PLAG1 in lipoblastoma, when myxoid
liposarcoma shows a t(12;16) (q13;p11) translocation [10-13].
Dilley et al. [14] had reviewed 24 patients who presented to a
single institution over a 15 year period. Of these 24 patients, only
4 had tumor in the head and neck region. The tumor may present
as a focal or diffuse lesion with the former being more common.
It has also been mentioned that focal lesions usually do not
require further surgery following initial resection. Patients with
lipoblastoma may present with various symptoms depending
upon its site. Rasmussen et al. [15], mentioned a case of cervical
lipoblastoma causing intermittent airway obstruction. Farrugia
et al. [16] reported another case of lipoblastoma of the neck
which was presented as a rapidly enlarging mass, mimicking
cystic hygroma. Eveline Bruyeera [6] reported three cases of
head and neck lipoblastoma. The outcome of three patients was
favorable after complete surgical resection. K Premkumar [2]
recently reported another case of an extensive tumor located over
the nape of the neck that causes a restriction of neck movement
Lipoblastoma exhibits a propensity to invade locally. If not
excised early, it may enlarge and infiltrate the various surrounding
structures. Various pressure symptoms may occur which can
lead to life threatening complications as noted hereinbefore [2].
The mainstay of treatment is complete non-mutilating
resection of the tumor to avoid recurrence. If the entire tumor
cannot be safely removed at the time of initial resection, a staged
approach is recommended. [17] The prognosis is excellent, and
the recurrence rate is less than 25% being largely attributed
to the infiltrative form ‘lipoblastomatosis’. The evolution is
unpredictable, spontaneous resolution and maturation into
lipoma may occur, but metastases still not reported so far [17,18].
Conclusion
Head and neck lipoblastoma are a rare childhood tumor,
usually presenting as a progressive painless mass, rarely causing
airway obstruction, nerve or vascular compression. Through our
case, we aimed to shed light on lipoblastomas as a differential
diagnosis of rapidly growing soft fatty masses of children within
this region.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about
juniper publishers: https://juniperpublishers.business.site/
Comments
Post a Comment