Extended External Auditory Canal Cholesteatoma: Case Report and Literature Review-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Introduction: External auditory canal
cholesteatoma (EACC) is a rare disease that manifests with unilateral
insidious chronic pain and otorrhea. Its evolution is slow and not very
symptomatic, and its diagnosis may be delayed. Hearing is usually
preserved. Computed tomography (CT) is recommended for all patients.
Treatment may be clinical or surgical.
Case report: Female, 69 years old, with
complaint of hypoacusis and right otorrhea 10 months ago. Otoscopy of
the right ear with epidermal debris in the external auditory canal and
intact tympanic membrane. Tonal audiometry showed moderate right mixed
loss. Temporal bone CT with expansive formation with soft tissue density
with insinuation to the external auditory canal on the right. MRI with
lesion presenting hypersignal at T2 and in the diffusion sequence, in
close contact with the sigmoid sinus. The patient underwent open
mastoidectomy. During the intraoperative period, facial nerve, sigmoid
sinus, jugular bulb, posterior and middle fossa meningeal exposures were
observed. Patient progressed well, without facial paralysis or
recurrence of the disease.
Discussion:This work calls attention to a
case of EACC with extensive invasion of the mastoid at the diagnosis.
The diagnosis of the lesion was clinical. CT and MRI aided in the
differential diagnosis. EACC, due to its insidious nature and anatomical
correlation with noble structures, should always be remembered in the
differential diagnosis of external auditory canal lesions.
Keywords: Cholesteatoma; External auditory canal; External auditory canal cholesteatoma
Cholesteatoma is usually defined as the presence of
skin in the middle ear cavity, that is, it consists of an external
matrix formed by stratified keratinized squamous epithelium on a
perimatrix of fibroconective tissue. It has lithic and migration
characteristics and can cause erosion of adjacent bone structures.
Traditionally, it is classified as congenital and acquired (primary and
secondary), depending on its etiology [1].
External auditory canal cholesteatoma (EACC) presents
uncertain etiology, representing an invasion of the squamous epithelium
associated with erosion in a localized area of the external auditory
canal (EAC). Several theories have been presented to try to explain the
aetiology and pathogenesis of this disease: localized periostitis,
chronic inflammation of the EAC, failed spontaneous elimination of
desquamated epithelial cells and dehiscence of the petrotympanic
fissure[2,3]. Smoking and small traumas in the ear canal may also
predispose its onset [2] and there are described cases of EACC
post-radiotherapy, probably due to tissue degradation with eventual
radionecrosis, impairing normal collagen synthesis and cell production
[4].
It is a rare disease, with an estimated incidence of
1.2: 1,000 new patients seen in otologicalpractice [5]. The first
author to
describe the manifestations of the EACC was Toynbee in 1850 [6]. It
occurs mainly in the population over 40 years old and manifests with
unilateral insidious chronic pain and otorrhea. In a review of 48 cases,
otalgia was the predominant symptom and frequently related to extension
to nearby structures [2].
Thus, the diagnosis is eminently clinical. When
examining otoscopy, the tympanic membrane is intact in most cases with
erosion restricted to one point of EAC [7]. Hearing is usually
preserved.6 Since the evolution is slow and not very symptomatic, its
diagnosis can be late, evolving with progressive bone destruction and
involvement of important neighboring structures (lateral sinus, facial
nerve, posterior fossa). Computed tomography (CT) is recommended for all
patients, on suspicion of EACC [3,8].
The differential diagnosis of EACC is made with
necrotizing external otitis, tumors and keratosis obliterans. Keratosis
obliterans, unlike EACC, is more frequent in young adults with severe
otalgia and bilateral conductive hearing loss, and the EAC is filled
with a keratin plug which when removed reveals a narrow, hyperemic and
granulating tissue. In EACC, the lesion usually presents as an epidermal
diverticulum in the inferior wall of the canal, filled by epidermal
debris and otorrhea, the
rest of the EAC is normal [7].
The treatment of EACC can be clinical or surgical. The first
is performed through local cleaning and topical antibiotic
application. The second is based on the removal of cholesteatoma
and necrotic bone. Most studies show that minor lesions can
be treated conservatively or by minor procedures under local
anesthesia, whereas larger lesions require a surgical procedure to
remove the cholesteatoma [2]. The following surgical indications
are considered: chronic pain (despite clinical treatment);
constant infection (due to the possibility of developing
bacterial resistance); the onset of facial paralysis or chronic
vertigo; progression of the lesion during follow-up; CT showing
involvement of the hypotympanum, jugular dome or mastoid;
Diabetes Mellitus or immunosuppression (predisposition to
necrotizing otitis externa) [7].
Patient R.M.L.A., female, 69 years old, attended the
Otorhinolaryngology outpatient clinic of the State Hospital of
Diadema with complaint of hypoacusis and intermittent otorrhea
on the right ten (10) months ago. She denied otalgia or dizziness.
Otoscopy of the right ear showed an accumulation of epidermal
debris in the external auditory canal, which when removed
revealed an intact tympanic membrane. The left otoscopy was
normal. Tonal audiometry showed moderate right mixed loss
(Figure1).
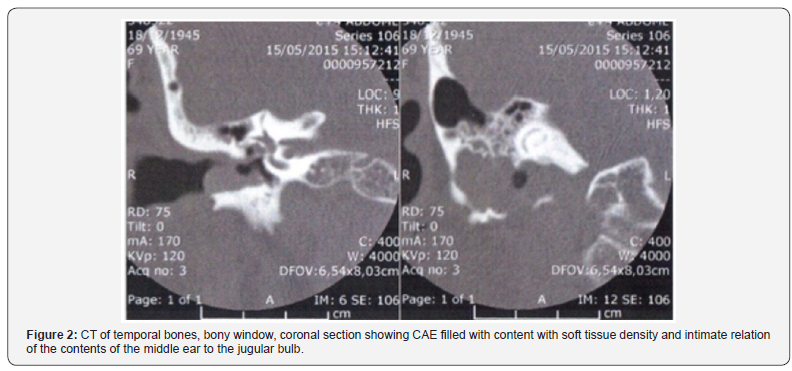
In the suspicion of cholesteatoma of the external auditory
canal, CT was requested of temporal bones, evidencing an
expansive formation with density of soft parts of inaccurate
limits, in the posterolateral region of the right mastoid, widening
the jugular foramen on this side, associated with component
lithium bone, gaseous foci of permeation and cortical rupture of
the anterior region of the mastoid, with an insinuation to the EAC
on this side (Figure 2).
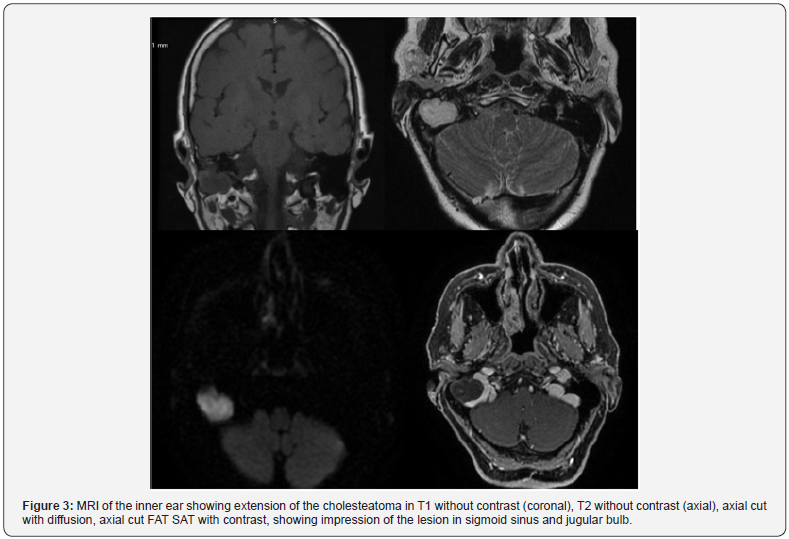
Magnetic resonance imaging (MRI) was used for differential
diagnosis, which showed an expansive lesion in the posteroinferior
portion of the right mastoid, with lobulated contours,
which penetrated the jugular foramen and CAE on this side.
The lesion presented hypersignal at T2 and in the diffusion
sequence and discreet peripheral enhancement of its superlateral
component. In addition, it had an intimate contact with
the sigmoid sinus and determined the extrinsic impression of
this sinus and the upper third of the right jugular vein (Figure 3).
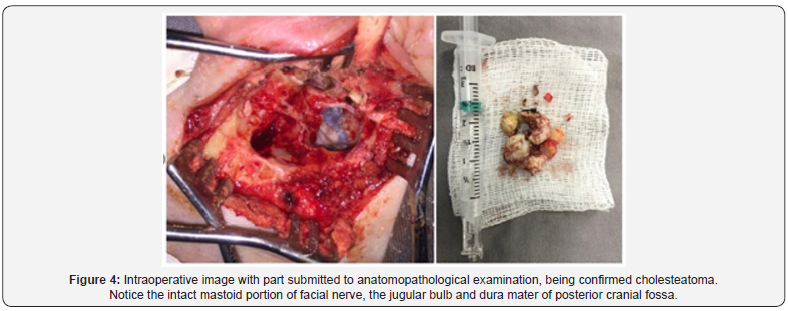
The patient underwent open mastoidectomy with
preservation of the antrum due to the absence of disease
in this region and as a way of avoiding a large cavity. In the
intraoperative period, the exposure of the sigmoid sinus, jugular
bulb and pre-sigmoid meningeal of the posterior fossa was
observed. Identified facial nerve exposed from the rope branch
of the eardrum to its exit at the tip of the mastoid, preserved
without trauma (Figure 4).
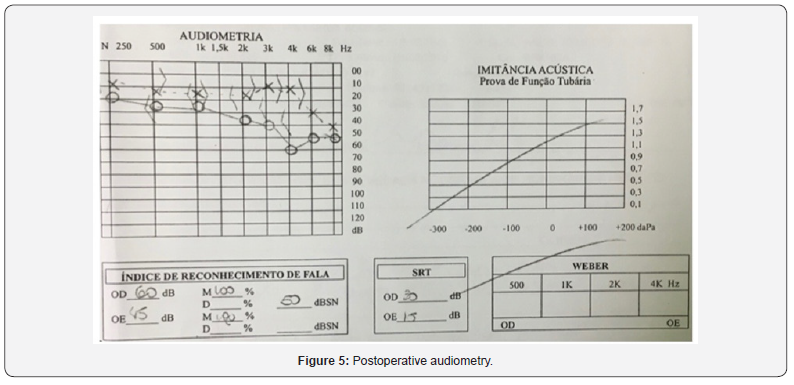
The patient progressed well, with no signs of peripheral
facial paralysis, without auditory threshold worsening (Figure
5) and no recurrence in the 10-month postoperative period.
Discussion
The EACC is a rare condition that presents with insidious
symptoms, while the extent of bone destruction progresses. In
the presented case the lesion was extensive at the time of its
diagnosis, compatible with the majority of cases in the literature,
diagnosed late [2,7,9].
Considering that the etiology of secondary EACC can be
explained, the origin of primary EACC remains uncertain. No
etiologic factor was identified in this case, so it can be considered
as idiopathic EACC.
Regarding the symptoms, the patient denied otalgia, different
from the cases found in our review of the literature [2,7,9].
The surgical procedure was indicated by the appearance of
the lesion and the patient’s lack of restrictions to perform it,
and the open mastoidectomy was performed, obtaining success
and ensuring a good control of the disease in the postoperative
period.
The involvement of the facial nerve pathway and the presence
of sigmoid sinus dehiscence and posterior fossa meninges could
be the cause of intraoperative complication or postoperative
sequela, however there were no intercurrences during the
procedure. The patient also did not present auditory sequela due
to the procedure.
As a form of postoperative follow-up of the lesion, in
addition to adequate cavity control and attention to the patient’s
symptoms, in the suspicion of residual cholesteatoma, it is
possible to perform MRI with diffusion [10].
a) Although rare, attention should be paid to the diagnosis
of EACC in cases of chronic otorrhea associated with otalgia
without changes in the tympanic membrane.
b) All patients should undergo temporal bone CT scans to
assess the extent of the injury as well as the involvement of
adjacent structures.
c) Surgical treatment in most cases is the indicated and
has shown good results in the removal and control of the
disease.
I would like to thank to all people involved & who supported
this study.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
Comments
Post a Comment