Cochlear Endoscopy in Cochlear Implantation of a X-Linked Stapes Gusher Syndrome-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
A 12-year-old boy with a five-year history of
bilateral sensorineural hearing loss and X-linked stapes gusher syndrome
developed progressive left-sided hearing loss. The pre-operative
computed tomography of the temporal bone showed a bulbous internal
auditory canal with a dysplastic cochlea and no apparent modiolus. A
1.3mm salivary endoscope was placed at the cochlear entrance to assess
the intracochlear anatomy. This revealed membranous structures of the
cochlea without direct communication to the internal auditory canal. We
advocate for the use of cochlear endoscopy to better delineate inner ear
anatomy, which will influence the implant selection and potentially
hearing outcomes in patients.
Keywords:MCochlear endoscopy; Otoendoscopy; X-linked stapes gusher syndrome; Cochlear implant; Perilymphatic gusher.
X-linked stapes gusher syndrome (otherwise known as
X-linked deafness type 3 or Nance deafness) is a rare form of
sensorineural hearing loss (SNHL) syndrome. Inherited in a sex-linked
recessive manner, it is believed to be the consequence of a
loss-of-function mutation on the X-chromosome in the POU3F4 gene at the
DFN3 locus [1,2]. Males tend to present greater phenotypic severity than
females, who present less frequently [3-5].
Affected patients have an abnormal configuration of
the lamina cribrosa and internal auditory canal (IAC) [1,3,4,6,7]. This
malformation leads to increased perilymphatic pressure and to stapes’
footplate fixation, giving rise to conductive hearing loss and
progressive cochlear nerve incompetence. This is relevant for surgeons,
as it results in an increased risk of perilymph gusher with surgical
manipulation [1,3,4,6,7]. This may lead to other complications, such as
otorrhea, rhinorrhea, and recurrent meningitis [8]. Meningitis
complicating cochlear implantation (CI), occurs at a higher rate in
patients with inner ear (IE) abnormalities, including X-linked gusher
syndrome [3,9].
Traditional approaches to imaging for CI utilize
computed tomography of the temporal bone (CT TB) and/or magnetic
resonance imaging. We report a case whereby intra-operative
otoendoscopic visualization allowed for real time visualization of the
IE anatomy, which allowed us to optimize our electrode
choice for CI. In this case, such visualization was valuable, as it
indicated the presence of the membranous portions of the IE to evaluate
if the modiolus was present, which we believe implied that a directional
electrode was the most appropriate choice.
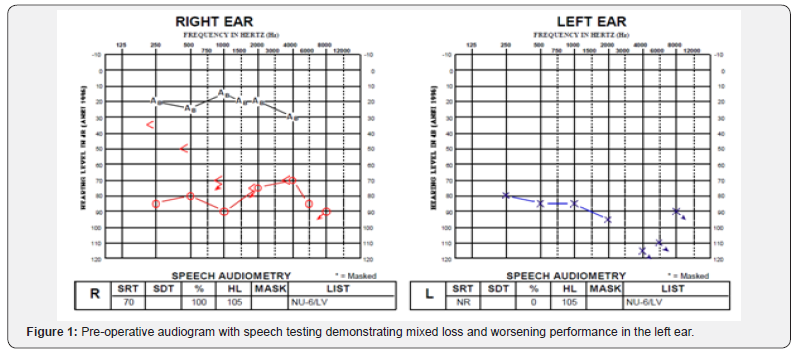
A 12-year-old boy with a five year history of
bilateral SNHL and X-linked stapes gusher syndrome presented with
progressively worsening left-sided hearing loss. He was initially
performing well with bilateral traditional hearing aids but developed
progressive mixed loss and worsening performance in his left ear. His
preoperative audiogram can be seen in Figure 1. He was sent for CI
candidacy assessment and was deemed to be suitable.
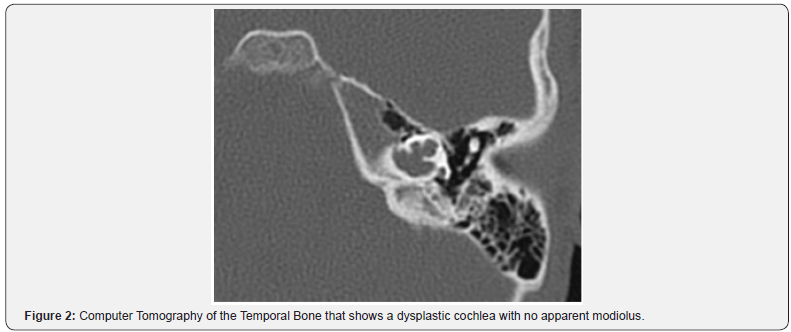
The pre-operative computed tomography (CT) of the
temporal bone was assessed. This showed a bulbous IAC with
a dysplastic cochlea and no apparent modiolus (Figure 2).
A CI24RE (ST) implant was initially selected by the implant
team due to the uncertainty regarding the location of the spiral
ganglion cells.
A 1mm cochleostomy was made anteroinferior to the
round window (RW). Upon entering the cochlea, a moderate
perilymphatic gusher was encountered. A 1.3mm rigid salivary
endoscope (Karl Storz, Germany) with a 3-chip full HD camera
head (Image1 S H3-Z) was approached trans-tympannically and
was placed at the edge of the 1mm cochleostomy to assess the
intracochlear anatomy.
To avoid injury to the inner ear, the CSF was not suctioned.
The same view was not achieved with the microscope as the
endoscope provided a more magnified and higher definition
view of the modiolus. There was evidence of membranous
structures of the cochlea without direct communication to the
IAC. Full insertion was achieved on the first attempt without
any difficulty and the gusher was controlled with packing of
periosteal tissue at the cochleostomy site. An intra-operative
plain X-ray confirmed the electrode placement.
When the cochlear modiolus and osseous spiral lamina
are
deficient, the absence of a bony septum creates a common space
seen on the imaging study [10] (Figure 2); there is an abnormal
communication between the IAC and the vestibule responsible
for the periphymphatic gusher. Patients with IE anomalies may
have both atypical positions of their spiral ganglion cells (SGC)
and have a higher likelihood of having fewer spiral ganglion cells
[11]. This has functional implications because at least 10,000
functional SGNs are necessary for effective speech discrimination 12].
Also this number can be further reduced by surgical trauma
[12]. Therefore, choosing the proper electrode device, namely, a
directional or a full banded electrode can help reduce the number
of lost SGNs. The fully banded CI electrode may be more useful in
the absence of a modiolus to allow for full and multi-directional
stimulation, whereas the pre-curved directional electrode may
be more appropriate if there is a modiolus present for precise
stimulation [13].
The proper electrode choice may have important hearing
outcome implications for patients with IE anomalies following
CI due to the challenges of reaching an optimal level of cochlear
stimulation, decreased dynamic range, a wider pulse width,
and weakened neural synchrony [7]. The functionality of CI is
correlated to the number of SGCs and their distances from the
stimulating electrode [14].
In our patient, we assumed that there was no IAC
communication due to the presence of modiolus. The moderate
CSF gusher was presumed to be secondary to his X-lined stapes
gusher syndrome and his enlarged IAC. Perilymph gusher during
CI in patients with X-linked gusher syndrome is inevitable, but a
thorough examination of the IE is still critical. CT of the temporal
bone is important for surgical planning, and it is also useful to
assess the likelihood of perilymphatic gusher [4]. Distinguishing
features on imaging include an enlarged bulbous IAC, a widened
cochlear aperture without the lamina cribrosa, cochlear
hypoplasia with modiolar deficiency, and a broadening of the
bony canal for the labyrinthine portion of the facial nerve [6].
Enlarged vestibular aqueducts may also appear in conjunction
with modiolar deficiency [15].
The rarity of X-linked gusher syndrome may result in
radiologists failing to recognize these signs, which may mislead
surgeons to perform stapedectomies that are otherwise
contraindicated. Thus, Incesulu et al. [3] advocated for high
resolution CT of the temperal bone to assess for congenital
dysplasia with ¬at least 1-mm thick slices [as opposed to 2mm
thick slices], which should ideally be assessed by an experienced
neuroradiologist [3]. Quan et al. [16] proposed that CT virtual
endoscopy should be done to evaluate CT data through threedimensional
reconstruction [16]. Limitations to both modes
of assessment assume that the CT images correlate perfectly
with the anatomy of the IE and that consistent radiological
consultation will occur. Our case, however, demonstrated that
intra-operative endoscopic findings do not always correlate with
CT findings, indicating that cochlear endoscopy may be a useful
tool to better delineate the intracochlear anatomy.
The otoendoscopic intracochlear view gave us accurate and
real-time information on the anatomy of the IE, which confirmed
the presence of a modiolus and the confidence that the CI would
not be in the IAC. This has the potential to allow us to make a
better-informed decision regarding the type of electrode to place.
Electrode choice is significant for patients with IE
abnormalities, since the location of neural tissue may be
abnormal. In patients that have an absent modiolus, a
circumferentially stimulating electrode may be preferred over
a full-banded electrode, which may risk adverse facial nerve
stimulation [3]. One explanation for post-operative facial nerve
stimulation in children with IE abnormalities is the close vicinity
of the electrode to the nerve [14]. Therefore, to avoid injury, the
proper choice in electrode should be made.
While CT temporal bone has served as the conventional
approach to assessing the anatomy of the IE, fthe endoscope
offers better resolution of the modiolus than the CT temporal
bone, as the CT indicated that there was no modiolus. We
advocate the use of intracochlear endoscopy in selected cases as
it offers a better resolution than even high-resolution CT. With
the potential to change electrode choices in CI, the customization
of electrode choice based on the presence of membranous IE
anatomy may change the hearing outcome of the patients with
anomalous IE anatomy and patients with uncertain location of
spiral ganglion cells.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
To know more about juniper publishers: https://juniperpublishers.business.site/
Comments
Post a Comment