Submental Endotracheal Intubation: A Useful Alternative-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Submental endotracheal intubation is a simple, useful
and safe technique in maxillofacial trauma when oral and nasal
endotracheal intubation cannot be performed. It prevents need for
tracheostomy and its consequent morbidity. Airway management in patients
with panfacial trauma is challenging due to disruption of components of
upper airway. Most patients have associated nasal fractures where use
of nasal route of intubation contra-indicated. Intermittent
intra-operative dental occlusion is needed to check alignment of the
fracture fragments, which contraindicates the use of orotracheal
intubation. The anesthesiologist has to share the airway with the
surgeons. Submental intubation provides intra-operative airway control,
avoids use of oral and nasal route, with minimal complications.
Submental intubation allows intra-operative dental occlusion and is an
acceptable option, especially when long-term postoperative ventilation
is not planned. This technique has minimal complications and has better
patients and surgeons acceptability.
Introduction
Francisco Hernandez Altemir in 1986 first reported
Submental intubation. According to him, it's a procedure that avoids
tracheotomy and allow for the concomitant restoration of occlusion and
reduction of facial fractures in patients ineligible for nasotracheal
intubation [1].
This procedure consists of exteriorizing an oral endotracheal tube
through the floor of the mouth and submental triangle. The surgical
procedure involves a 2cm incision in the Submental, paramedial region
extending cephalad until the lingual mucosa was tented with a hemostat
after which another 2 cm incision parallel to the mandible is made in
the lingual gingiva. The breathing circuit is briefly disconnected as
the tube is externalized through the Submental region and reconnected to
the circuit and secured to the patient. Submental intubation is a
surgical adjunct in facial trauma, pathology and elective facial
surgery.
Oral intubation interferes with maxillomandibular
reduction. In situations where maxillomandibular fixation is required
and nasoendotracheal intubation is contraindicated, cricothyrotomy or
tracheostomy has been the traditional method of airway control [2].
Submental intubation technique consists of passing the tube through the
anterior floor of mouth, allowing free intra-operative access to oral
cavity and nasal pyramid without endangering patients with skull base
trauma. Submental intubation can be used when short term postoperative
control of airway is desirable with the presence of undisturbed access
to oral as well as nasal airways and a good dental occlusion.
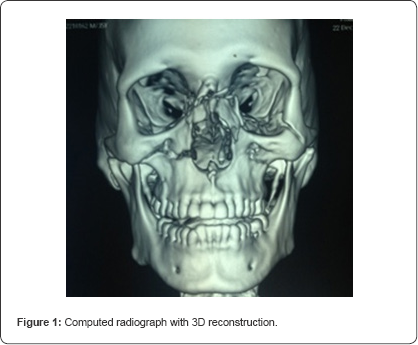
A 35 year old male patient with 70kg weight met with a
road traffic accident and was admitted to hospital. On admission
patient was conscious with a Glasgow coma score of 15. On examination,
there was facial swelling, laceration at Naso-orbito- ethmoid region and
epistaxis was present. There was tenderness at zygomatic buttress
region and mouth opening was restricted. Radiological examination
revealed Nasal bone fracture with presence of high Lefort I fracture on
the right side (Figure 1).
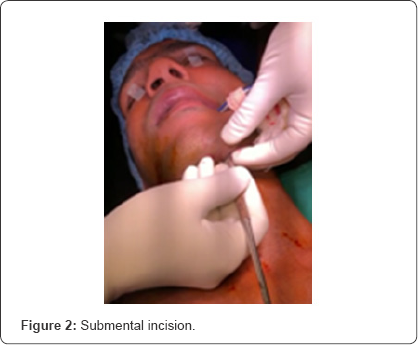
The patient was scheduled for surgical correction of
multiple facial fractures. Nasal endotracheal intubation was
contraindicated in the presence of nasal bone fracture. Oral
endotracheal intubation was not possible because the surgical procedure
involved intraoperative intermaxillary fixation to obtain occlusion. In
order to avoid tracheostomy, submental endotracheal intubation was
planned. Patient was kept fasting for 8 hours preoperatively. He was
premedicated in preoperative room and then in operation theatre was
preoxygenated with 100% oxygen for three minutes. A 2cm incision was
made in left submental region parallel and medial to inferior border of
mandible by the surgeon (Figure 2).
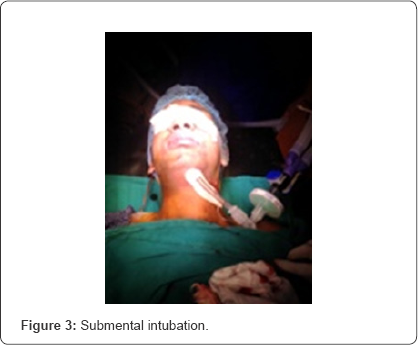
It was extended intraorally through the mylohyoid
muscle by blunt dissection. The endotracheal tube was briefly
disconnected from the breathing circuit and the tube connector was
removed from the tube. The pilot balloon followed by endotracheal tube
was gently pulled out through the incision. The tube connector was
re-attached and the endotracheal tube reconnected to an aesthesia
breathing circuit (Figure 3).
Bilateral air entry was rechecked and found to be
equal and the tube was fixed with 1'0 silk suture. Intraoperatively, the
endotracheal tube was away from the surgical field and the surgeons
could easily do the intermaxillary fixation to check occlusion. The
total duration of surgery was five hours. At the end of surgery,
submental intubation was converted to oral intubation. First the pilot
balloon and then the endotracheal tube were pulled intraorally. The
submental incision was closed using two skin sutures so as to allow
certain degree of drainage. Patient was extubated uneventfully. After
two months, submental scar was almost invisible.
Discussion
Submental intubation is a simple, secure and
effective procedure for operative airway control in maxillofacial trauma
surgery. It allows surgeons to avoid the risk of epistaxis, iatrogenic
meningitis or trauma of the anterior skull base after nasotracheal
intubation as well as complications such as tracheal stenosis, injury to
cervical vessels or the thyroid gland, subcutaneous emphysema, or
recurrent laryngeal nerve injury related to tracheostomy [3,4].
The scar from the submental incision is thought to be less visible than
a tracheostomy scar and is well tolerated by patients [5].
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment