Incidence, Recurrence and Complications after Facial Skin Cancer Excision: Retrospective Analysis of Multi-Institutional Experiences-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Objectives: Skin cancer varies in incidence
according to Geography, sun exposure, genetic predilection, skin type
and many other factors. Definite treatment of skin cancer requires
multidisciplinary approach. Surgery is usually giving a strong hand in
skin cancer management regardless to the size of the lesion. This study
is designed to evaluate the incidence, recurrence and complications in
patients, who had undergone facial skin cancer excision then
reconstruction.
Material and Methods: Retro analysis review
was conducted for the complications that had happened in patients who
were having facial skin cancer and underwent excision then
reconstruction. Of 254 cases, 54, 25 and 175 cases were submitted to
direct skin closure, skin grafts and local facial flap reconstruction
respectively
Results: The total reconstructive surgery
complications in this study were in 16 cases of254 (appx. 6.3% of the
study). Most of surgical reconstructions are carried out by local facial
flaps with good outcomes. Total skin cancer recurrences had been
reported in 5 cases (appx. 2.5% of the study).
Conclusion: Incidence of skin cancer in sunny
countries like Egypt, where there is a cumulative effect of the sun,
moves towards nonmelanoma skin cancer. Local skin cancer recurrence in
these series is about 2.4%. Different surgical reconstructive modalities
areused, including direct simple closure of the wound, skin grafting
and local facial flaps. The commonly used flaps for face reconstruction
after excision of skin cancer, in this study, are advancement flaps,
naso-labial flaps and forehead flaps with the same survival
potentiality.
Keywords: Skin cancer; Reconstruction; Complications; Recurrence
The most common facial skin cancers are Melanoma, basal cell carcinoma and squamous cell carcinoma [1,2].
Different incidences are recorded according geographical and genetic
factors. Surgery has an important role in treatment of facial cancer [3].
Surgical reconstructive options are usually available and different
according to many parameters as the defect size and site, patient
general condition and surgeon’s experience caliber.
Materials and Methods
Retro review analysis was conducted for the
complications that happened to patients who were having facial skin
cancer and underwent excision then reconstruction. The study was
included through multi institutional data and analyzed regards surgical
complications. 254 patients were included in the study during the period
from January 2014-2017. 254 cases were managed by surgical excision and
included in the study. Small defects less than 2cm*3cm were closed
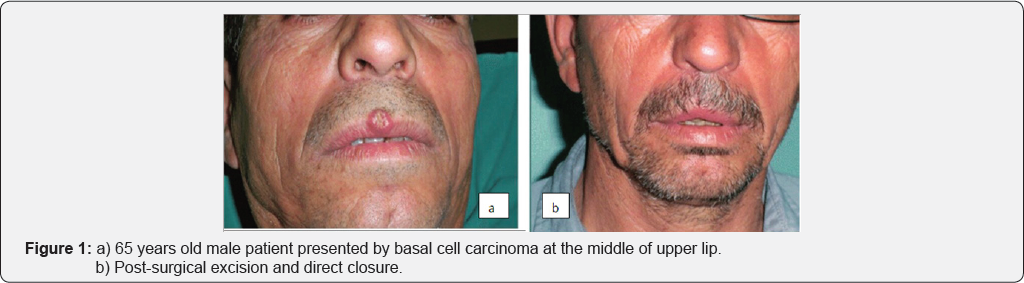
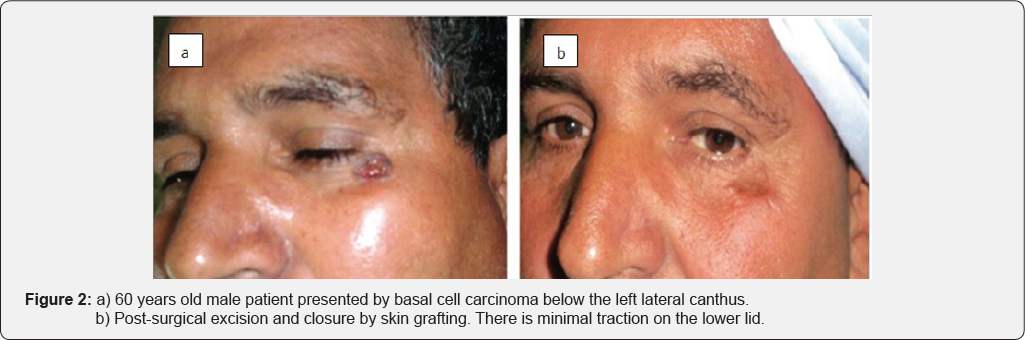
directly in 54 cases, after lesion excision (Figure 1a & 1b). Larger post-surgical defects were closed by skin grafts (Figure 2a & 2b) or local skin flaps (Figure 3a & 3b) in 25 and 175 case respectively. Flap reconstruction was achieved by one of the three commonly used local facial flaps [3].
Advancement flaps by one of its different patterns, transposition or
rotational flaps and Nasolabial flaps were proceeded in 80, 10, 52 case
respectively.

Facial cancer was distributed in different incidence
presentations in facial areas; 81 case in the nose, 35 case in upper
lip, 19 case in lower lip, 24 case in check inferior and medial to
lateral canthus, 21 case inferior and lateral to medial canthus, 23 case
at forehead, 14 case at scalp area, 22 case at the mandibular margin
and 15 case at pre-auricular area. Sentinel and draining lymph nodes
were free by clinical examination and investigations.
Of 254 patients were presented by skin cancer in the
face, 205 were due to basal cell origin, 45 were due to squamous cell
and other non-melanoma cancers. Only 4 cases of skin cancer in the study
were due to melanoma. Average patients' age is ranged from 35-75 with
mean age of 55 years. Male patients were 159 and 95 were females, aged
from 35-75 year. Multi-centric data were collected from Sayed Galal,
Al-Hussein, Nasser Institute and AL-Harm hospitals, Cairo, Egypt.
Informed consent for surgery, any possible complications and photography
were signed by each patient. Study was approved by my institutional
ethical committee.
The total incidence, of reconstructive surgery
complications, is 16of 254 (app 6.3%.of the study). The Complications
have been varied in different presentations according to type of
reconstructive surgery. Of 54 cases were closed directly, 2 cases showed
recurrence within two years postoperative. Of 25 cases were
reconstructed by skin grafting, one case howed retraction of the lateral
canthus with minimal scleral show (Figure 3)
and another case has recurrence of squamous cell cancer after 3 months
of surgery. Of 175 cases were treated by local facial flap
reconstruction, 11 cases were complicated by flap dehiscence. Flap
dehiscence underwent in 8 patients, who were reconstructed by
advancement flap, 2 were reconstructed by naso-labial flaps and one case
was reconstructed by median forehead flap.
Although all flaps have sensationally survived
without major wound healing complications, but edge dehiscence has been
recorded in 11 cases of 175 have been reconstructed by flaps. Total skin
cancer a recurrence was reported in 5 cases (appx 2.5% of the study).
Of 5 cases of recurrence, 3 were due to recurrent squamous cell cancer
and 2 were due to recurrent basal cell carcinoma. All recurrent cases
were re-operated with immediate reconstruction after frozen section
biopsy.
Surgical closure after facial skin cancer excision is
one of the main pillars in the treatment of small sized facial lesions
in head and neck. However surgical reconstruction is the first line in
treatment of large sized facial skin cancer. In most cases, surgery
should be done upon two stages, first one is excision and the second one
is reconstruction or wider excision, based on histological clearance
about lateral and deep resection margins and sometimes after
intraoperative frozen section assessment
[4].
These facts are correlated with this study, when
surgery was the mainstay in definite treatment. Large lesion more than 2
cm x 3cm defiantly needs post excision reconstruction. Reports about
histological incidence of skin cancer are ranging from 75-80% incidence
of non-melanoma skin cancer, according to skin cancer institute in North
America and cancer journal respectively [5,6].
In this study the incidence of non-melanoma skin cancer in head and
neck is 98.8%. Basal cell carcinoma has 80.7%, while squamous cell
carcinoma has 18.1% of the skin cancer incidence in our study, while it
is 22% in other worldwide statistics.
According to Cleveland clinic [7]
center for continuous education, they state that; new skin cancers will
be basal cell origin in about 80%, (BCC), squamous cell carcinoma in
16%, and Melanoma in 4%. This slightly differs from this study report
regards BCC and SCC. Although it is higher more than double folds,
regards Melanoma incidence.
This could be explained by the predisposing factor;
sun exposure, which has been mostly cumulative in non-melanoma skin
cancer and has been an acute exposure in melanoma one. So residents of
sunny countries, theoretically, where they are cumulatively exposed to
sun and more vulnerable for nonmelanoma skin cancer. Contradicted to
this peoples who lives in non-sunny countries, when exposed acutely to
the sun anywhere, they are at a risk to develop melanoma.
Meticulous surgery, facial units understanding,
relaxing skin tension lines and proper choice and design of the flap are
important factors in successful reconstruction after tumor excision
from the face. Facial flap surgery is an old finding in the Indian
civilization [8],
and it has been considered an early whispering of reconstructive
surgery in modern western literatures. In this study, three types of
flaps with their variant designs were used in 175 cases to reconstruct
defects after skin cancer excision from the face. Advancement flaps have
showed better aesthetic outcome than nasolabial and forehead flaps,
although all flaps have showed sensational survival.
This study reported 6.3% total incidence of
reconstructive surgery complications. Small defects are usually closed
directly if submitted to surgery [9].
Direct skin closure has incidence of 0.5%, while skin grafting has
showed 0.25%, but the two options are not applicable for large lesions
and when the lesion is present in special areas as medial canthus,
lateral canthus, and facial angles and when there is a bone or
cartilaginous exposure. Of 175 cases were treated by local facial flap
reconstruction, 11 cases were complicated by flap dehiscence. 8 cases
were reconstructed by advancement flap, 2 were reconstructed by
nasolabial flaps and one case was reconstructed by median forehead flap.
Flap complication reported also 6.3% higher than another study; it was
4.6% in Rao JK & Shende KS study [3]. Facial Flaps outcomes were extensively discussed in another author's article [10].
This study has showed the total skin cancer a
recurrence is 5 of 254 cases, (appx 2.5% of the total cases) and they
were subjected for reconstructive ladder. These results of recurrence
are lower than those recorded by Marri, et al. study [11]
which is 4.2%. This study is concerning facial skin cancer in face and
scalp only, not the deep cancers in head and neck as the study carried
out by Raj et al. in 2017 [12].
Recurrence occurred in 5 cases, 3 were due to
recurrent squamous cell cancer and 2 were due to recurrent basal cell
carcinoma. Aesthetic outcome is more satisfactory when advancement flaps
were used.
The incidence of skin cancer in face and scalp, at
sunny countries like Egypt, where there is cumulative effect of the sun
is higher towards non- melanoma skin cancer. Small skin cancer is easy
to be reconstructed after excision either by direct closure, skin graft
or local facial flaps. Larger lesions need definite flap reconstruction
after excision. The commonly used flaps for face reconstruction after
excision of skin cancer, in this study are; advancement flaps,
nasolabial flaps and forehead flaps with same survival potentiality.
However Aesthetic outcome is more satisfactory when advancement flaps
are used. Local skin cancer recurrence in these series is about 2.4%.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment