Tuberculous Otitis Media with Facial Palsy in Pulmonary Tuberculosis Treated Patient-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Tuberculous otitis media is relatively rare and often
masquerade as other common otological conditions resulting in delay of
diagnosis and complications of disease. It is usually characterized by
painless chronic ear discharge with multiple tympanic membrane
perforation and presence of abundant granulation tissues in the middle
ear on examination. We report the case of a 35 year old man who
presented with symptoms of acute otitis media secondary to
tuberculosis.
Introduction
Mycobacterium tuberculosis infection remains among the most insidious diseases worldwide [1].
Regarding extra- pulmonary M. tuberculosis infection, 95% of cases
involve the head-neck region (larynx, lymph nodes, tonsils, pharynx,
oral cavity, salivary glands, and external and middle ears) [2].
Tuberculosis is a chronic granulomatous infection that can infect any part of the temporal bone [3].
Tuberculosis affects the middle ear through three routes; aspiration of
mucus through the Eustachian tube, blood borne dissemination from other
tuberculous foci or direct implantation through the external auditory
canal and tympanic membrane perforation. Middle ear involvement in the
absence of active pulmonary disease is rare, but may occur. Facial
paralysis associated with chronic otitis media suggests a high
probability of cholesteatoma, and surgical intervention is appropriate.
The mechanism of facial paralysis associated with cholesteatoma may be
compression or inflammation.
We present a case of TOM in a patient with associated
facial palsy and healed pulmonary Koch’s lesions. The diagnosis was
made by clinical evaluation, radiography of the chest and
histopathology.
Case Report
A 35 year male presented in our opd with complaints
of left side purulent ear discharge for 3 months left sided facial
muscles weakness for past one month and dizziness for 20 days and
progressive diminution of hearing. It all started 5 years back when
there was left otalgia which followed with purulent otorrhea which got
relieved on taking medication. Patient complained of facial muscles
weakness for 1 month. There was history of dizziness for last 20 days
which relieved on medication.
Patient had completed antitubercular treatment under
category 1 regimen 2 years back following which his pulmonary symptoms
got relieved.
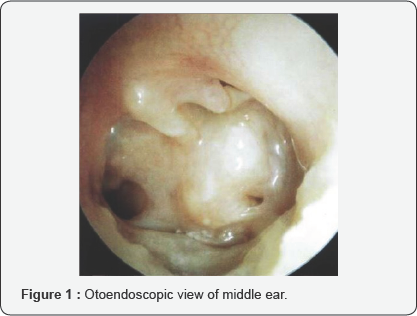
Otoendoscopic examination of the left year revealed
total perforation of tympanic membrane, characteristic pale middle ear
mucosa, metalized handle of malleus adherent to promontory and
hypotympanic air cells (Figure 1).
The right tympanic membrane was essentially normal. There was no
mastoid tenderness but Grade IV (House-Brackman score) facial palsy on
left side (Figure 2).

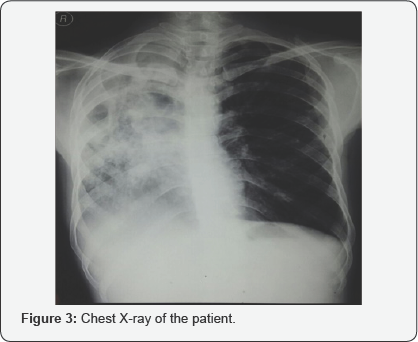
Audiometry shows severe to profound hearing loss in
left ear and moderate to moderately severe hearing loss in right ear. A
digital Chest X-ray revealed right sided healed tuberculous lesions with
calcifications and fibrosis (Figure 3).
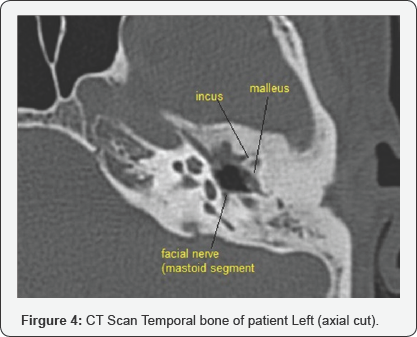
Monteaux test was positive and Faraday stimulation showed 4.5mA in
right ear and 9.5mA in left ear. CT scan temporal bone revealed
metalized handle of malleus and exposed mastoid segment of the facial
nerve (Figure 4).
Modified radical mastoidectomy was done and pale granulations and
fibrous tissues were seen, tegmen plate with a sheet of fibrous tissue
dehiscent of some bone was found. The pale granulations were sent for
histopathology examination.
Histopathology report of granulations showed
granulomas, composed of epitheloid cells, lymphocytes and occasional
giant cells i.e., consistent with tuberculosis [4,5].
He was commenced on antitubercular medications under Category 2 as per
Revised National Tuberculosis Control Program (RNTCP) and pulmonary
symptoms got improved.
Discussion
The occurrence of tuberculosis of the middle ear has
dramatically decreased, from about 1.3%-18.6% in the beginning of the
last century, down to 0.04% of all cases of chronic suppurative otitis
media according to a study report [3]. Wallmer [6]
first described clinical features of tuberculous otitis in 1953,
including painless otorrhea, multiple tympanic membrane perforations,
granulation tissue in the tympanic cavity and mastoid, and bone necrosis
with progressive conductive hearing loss and facial palsy. Varty et al.
[7] further asserted that the combination of surgery and medical therapy improves prognosis.
All authors agree that treatment of TOM, including
the nonlung-involving forms, has to include anti-TBC pharmacological
protocols for at least six months [8].
With regard to the role of surgical treatment, it should be considered
for the treatment of complications, such as subperiosteal abscesses, but
it is controversial in case of uncomplicated TOM [8].
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment