Tuberculosis of Cervical Spine-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Tuberculosis (TB) of spine is part of an
extrapulmonary tuberculosis manifestation and is the most common form of
skeletal tuberculosis. It affects mostly at the thoracic and lumbar
region owing to its blood supply but uncommonly spreads to the cervical
spine. This article describes a 67-year-old lady who presented with neck
pain secondary to TB of cervical spine.
Keywords: Tuberculosis; Spine; Cervical
Introduction
Cervical TB spine is particularly rare, representing 3-5% of all spinal TB cases [1].
Mainstay treatments are usually chemotherapy with long duration of
anti-tuberculosis medication. Only limited cases are indicated for
surgery in which anterior approach to cervical is more favorable [2].
Case Report
We introduce a case of a 67-year-old lady initially
presented in December 2016 with a complaint of neck pain radiating to
both shoulders which resolved with physiotherapy and analgesia. However,
she experienced worsening neck and interscapular pain in February 2017.
This was accompanied by reduction of weight and appetite. Examination
of the neck demonstrated localized tenderness to lower cervical and
upper back. ROM of the neck was reduced. No palpable cervical lymph
nodes were found. Neurological examination of the upper limbs and lower
limbs were unremarkable with intact power, sensory and reflexes
consistent with American Spinal Association (ASIA) Impairment scale
grade E.
Laboratory test revealed elevated Erythrocyte
Sedimentation Rate of 40mm/hr and C-Reactive Protein of 24mg/l. Sputum
acid fast bacilli (AFB) test and Mantoux test were both found to be
normal.
Cervical radiograph showed lytic destruction of
vertebral body of C6 and C7. MRI unveiled destruction of C6/C7
intervertebral disk, adjacent vertebral endplates erosion and spinal
stenosis at this level. There were no surrounding collection or
abscesses at this level. Chest radiograph did not show any nodular
lesions suggestive of pulmonary tuberculosis.
Patient was electively planned for surgery; anterior
cervical corpectomy of C6 and C7 with biopsy. She was positioned supine
with head in extended position. Shoulders were strapped and pulled with
minimal traction to allow visualization of the lower cervical on lateral
radiographs. A small towel was also placed in between the scapula to
drop the shoulders further.
The skin was prepared with povidone iodine,
disposable drapes and iodine impregnated dressing. A standard anterior
approach to the cervical was made from the left side of neck. The
pathological cervical and intervertebral disk of C6/C7 were removed by
piecemeal and its specimen sent for histopathological examination (HPE).
A Harms titanium mesh cage was implanted with autologous tricortical
iliac bone graft packed into it. An anterior cervical plate spanning C5
to T1 was then placed.
Discussion
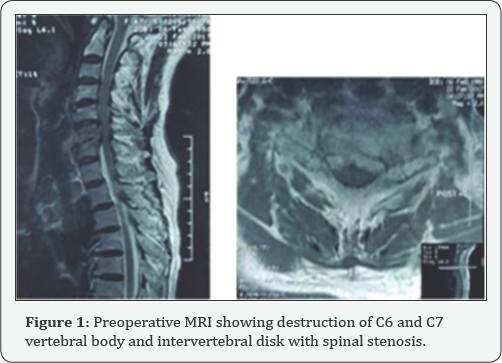
Tuberculosis is a great mimicker with multitude of
clinical features and presentations. Initial diagnosis in this case was
pyogenic (Figure 1 & 2)
spondylodisciitis in view of increase inflammatory markers but negative
sputum AFB and Mantoux test. It was the intraoperative HPE that
revealed granulomatous inflammation with infiltrate lymphocytes,
epitheliod macrophages and Langhans multinucleated giant cells which are
typical of Mycobacterium tuberculosis.

Tuberculosis is always secondary to a primary focus, often the pulmonary or genitourinary system [3].
TB spine is most commonly found in lower thoracic and upper lumbar
regions. The middle thoracic and cervical region is less frequently
involved. It commonly spreads by hematogenous dissemination of the bacillus
both via arterial or venous. Infection of the paradiscal area is from
the rich subchondral arterial plexus that is derived from the anterior
and posterior vertebral arteries [4].
Infection of the vertebral body however is associated with intraosseous
venous plexus derived from Batson paravertebral venous plexus. In most
adult cases, TB spine results from reactivation of resting tubercle
bacilli in quiescent lesions produced during an earlier infection.
Majority of TB spine are treated with
anti-tuberculosis medication. British Medical Council and the Cochrane
recommends treatment with appropriate anti- tuberculosis medication
noting that there is insufficient evidence for routine use of surgery [5].
Surgeries however, are indicated in cases with neurological deficit,
progressive deformity, pan vertebral lesions, and spinal TB that are
refractory to medical therapy [6]. Other indications are severe pain from sequestered bone and disc, expanding abscess or instability [7].
The increasing neck pain she was experiencing was a
result of destruction to the cervical spine giving rise to instability.
The goal of surgery was to eradicate infection, obtain tissue biopsy to
determine exact organism and provide stability.
In the Hong Kong procedure, the spine is approached
anteriorly so that the area involved are dealt with directly. It
provides best access for debridement, stabilization by grafting and
facilitates rehabilitation, thus considered as the standard operative
treatment when surgery is indicated [8,9].
Hassan et al reported satisfactory outcome of single
stage anterior autogenous iliac bone grafting and instrumentation in
lower cervical spine tuberculosis involving 16 patients [10].
12 showed complete recovery and 2 had marked improvements at an average
of 38 months. All patients experienced reduction in pain
postoperatively. Similarly, this patient had significant reduction in
pain score after surgery.
Conclusion
One third of world's burden of tuberculosis are still found in South East Asia [11].
Health providers must have high index of suspicion as clinical
presentation of tuberculosis are diverse. Mainstay treatment is
anti-tuberculosis medication with surgery indicated in few.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment