Symptomatic Outcomes of FESS-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
The term 'sinusitis’ refers to a group of disorders
characterized by inflammation of the mucosa of theparanasal sinuses.
Because the inflammation nearly always also involves the nose, it is now
generally accepted that ‘rhinosinusitis’ is the preferred term to
describe this inflammation of the nose and paranasal sinuses. Presently,
functional endoscopic sinus surgery (FESS) is the standard treatment of
chronic rhinosinusitis (CRS) and in sinonasal polyposis. The endoscopic
procedure is based on the principles introduced by Messerklinger, which
prioritize both the function and the permeability of pre-ethmoidal
spaces. In 1985, Kennedy described this technique and popularized the
term “Functional Endoscopic Sinus Surgery - FESS”.
Keywords: FESS; Chronic; Rhinosinusitis; Polyp
Abbreviation: FESS: Functional endoscopic sinus surgery
Introduction
Endoscopy of nose was first performed by Hirschmann [1]
in 1903 using a modified Nitzecystoscope which he used in the nasal
cavity and in the maxillary sinus via a tooth socket. In 1922, Speilberg
[2]
was the first to introduce an endoscope into the maxillary sinus via
the inferior meatus, but it was in 1925 that Maltz commissioned Wolf to
make a dedicated endoscope. These endoscopes using a series of small
lenses continued in use until Hopkins, Professor of Optics at Reading,
invented a far superior system in the 1950s, based on solid glass rods,
which is now universally in use. Presently, functional endoscopic sinus
surgery is the standard treatment of chronic rhinosinusitis (CRS) and in
sinonasal polyposis. The endoscopic procedure is based on the
principles introduced by Messerklinger, which prioritize both the
function and the permeability of pre-ethmoidal spaces. In 1985, Kennedy
described this technique and popularized the term “Functional Endoscopic
Sinus Surgery - FESS”.
Methodology
This study includes 52 patients who underwent
functional endoscopic sinus surgery and consented for participation in
the study. Out of 52 patients, 32 patients were diagnosed with sinonasal
polyposis and 20 patients were diagnosed with chronic rhinosinusitis
(CRS). We excluded recurrences and reoperation cases. The diagnosis of
both pathologies was clinical as well as radiological. Medical treatment
was attempted for CRS. All patients of CRS were given preoperative
medical management with antibiotics and topical steroids for atleast 12
weeks.
All the endoscopic procedures were carried out under
general anesthesia. The surgical technique described by Messerklinger
and Stammberger was used. All the patients included in the study signed a
valid written informed consent explaining the needs and goals of the
study. All the patients of nasal polyposis were given preoperative
corticosteroids and antibiotics intravenously atleast for 3 days.
Injection 2 percent lignocaine (with 1:80,000) adrenaline was used for
local infiltration. Post-operatively nasal packing of all the patients
with Merocel pack was done which was removed after 36 hours. Average
hospital stay was 5 days, with post-operative follow up at 7, 15, 30
days, and at 6 months. Antibiotics and steroids were continued post-
operatively and the patients were given nasal douching vigorously with
0.9% saline solution in their noses. Topical steroids was started 5 days
after the procedure, and continued if necessary. Nasal cleaning and
crust removal were carried out in the post op follow up.
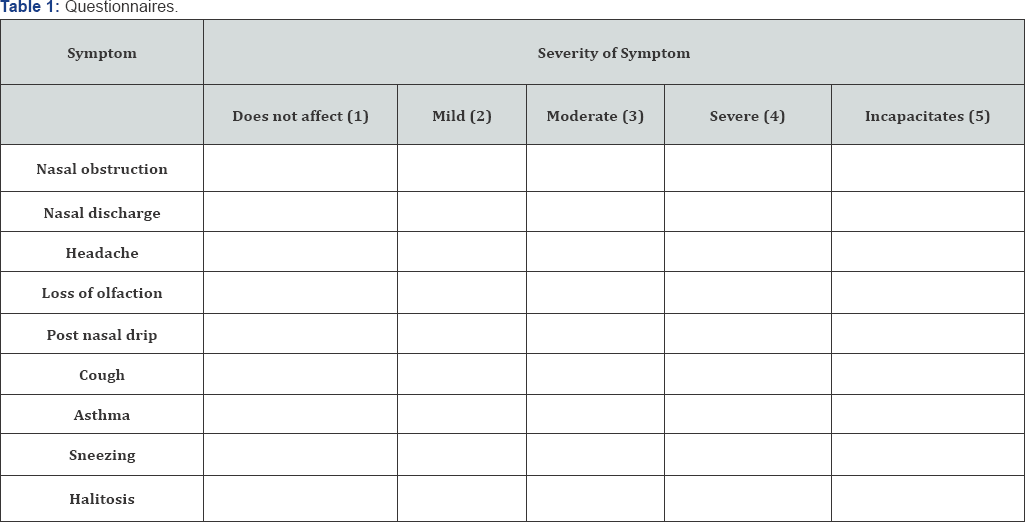
All these patients answered questionnaires about
their symptoms before and after surgery. All the questions were in
simple language for better understanding of the patients. Each answer
was scored from 0 to 5 according to Likert's scale. In order to analyze
the data, we considered good surgery outcome when the score difference
between pre and postoperative symptoms for each symptom resulted in a
positive value equal or above 2. If the difference resulted in a
negative value, equal or above 2, the procedure was considered a
failure. In cases which the score difference between pre and post op
were between +1 or -1, we concluded that the procedure did not influence
a certain symptom (Table 1).
Results
Of all the patients who answered the questionnaire,
28 were male and 24 were female, belonging to age group 07-58 years.
They were then separated in two groups, the ones of chronic
rhinosinusitis (CRS) alone were 20 in total and those with chronic
rhinosinusitis (CRS) and polyp were 32. As for symptomatic health
improvement after the procedure, both groups reported excellent outcome.
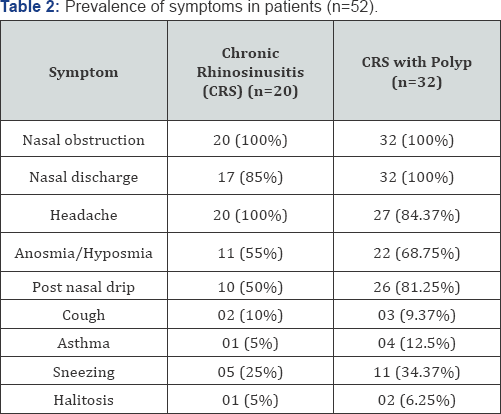
Table 2 lists the prevalence of symptoms reported by patients with CRS and CRS with polyp. Table 2 depicts the results obtained through FESS. (Table 3)
Discussion
The term 'sinusitis' refers to a group of disorders
characterized by inflammation of the mucosa of theparanasal sinuses.
Because the inflammation nearly always also involves the nose, it is now
generally accepted that 'rhinosinusitis' is the preferred term to
describe this inflammation of the nose and paranasal sinuses. A widely
accepted set of classifications or definitions was developed by the
Rhinosinusitis Task Force of the American Academy of Otolaryngology-Head
and Neck Surgery [3] and reported by Lanza & Kennedy [4].
These criteria are based in large part on temporal time frames. The
distinctions between acute rhinosinusitis (ARS), recurrent acute
rhinosinusitis (RARS), subacute rhinosinusitis (SRS), chronic
rhinosinusitis (CRS) and acute exacerbation of chronic rhinosinusitis
(AECRS) are based on the temporal differences in the presentation and,
in some cases, on the clinical presentation. There are also differences
in the histopathology and the bacteriology of acute and chronic
rhinosinusitis [4].
The major symptoms are nasal obstruction, facial pain/pressure, facial
congestion/fullness, rhinorrhea and hyposmia and the minor symptoms are
headache, dental pain, halitosis, fatigue, dry cough, fever and earache.
2 major symptoms, one major and 2 minors or purulent discharge in the
nasal cavity suggest CRS [5].
The mechanisms behind polyp formation are believed to be
multifactorial. A variety of environmental and genetic factors play a
role in the pathogenesis of inflammatory polyps and the role of
proinflammatory cytokines, chemokines, and chemotactic mediators is
increasingly being appreciated [6] (Table 4).

Nasal endoscopy and imaging were not used in this
study to quantify the clinical management of chronic rhinosinusitis
because chronic rhinosinusitis is a symptom-based condition, and
symptom-free patients usually does not require additional treatment,
even when they present minor alterations in endoscopic examination or
mucosal thickening in CT scans of the paranasal sinuses.
Nasal obstruction, rhinorrhea and headache are the
CRS symptoms that most impact patient's quality of life. In our study,
these were also frequent complaints. Nasal obstruction was present in
100% of the patients, rhinorrhea in 94.23% and headaches in 90.38%.
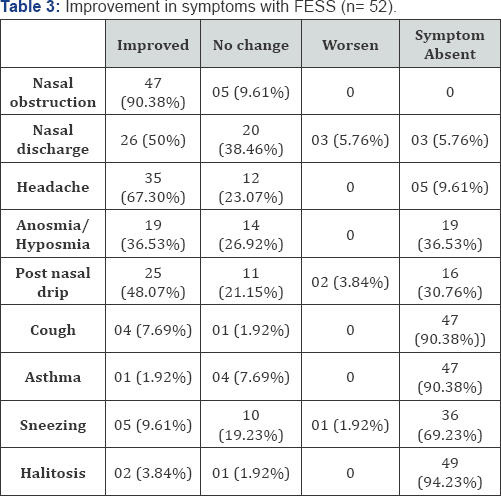
In present study, symptoms that had the most
improvement after surgery were nasal obstruction (90.38% improvement)
followed by headache (67.30% improvement) and nasal discharge (50%
improvement). Polyp patients had a trend of presenting with greater
symptoms relief after surgery.
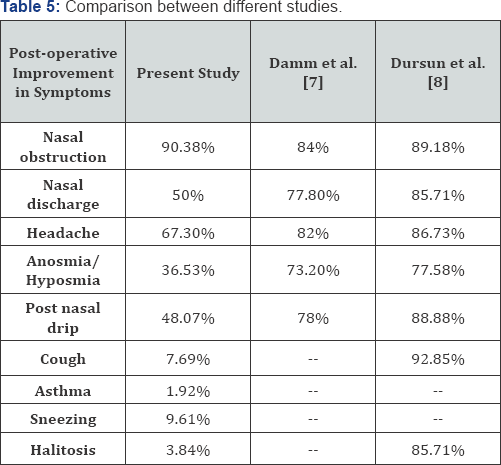
Damm et al. [7]
observed improvements of 84% in nasal obstruction, 77.8% in rhinorrhea,
82% in headache, 78% in post nasal drip and 73.2% in hyposmia after
sinus surgery.
Dursun et al. [8]
observed improvements of 89.18% in nasal obstruction, 85.71% in
rhinorrhea, 86.73% in headache, 88.88% in post nasal drip and77.58 % in
hyposmia after sinus surgery (Table 5).
Conclusion
The objective of this study was to determine if patients undergoing
functional endoscopic sinus surgery (FESS) obtain significant
symptomatic benefit from surgery. The leading complaints within the
symptomatic profile of patients with chronic rhinosinusitis are nasal
obstruction, nasal discharge and headache. The restriction of quality of
life in patients with chronic rhinosinusitis is mainly caused by these
symptoms, which can be improved in excellent fashion by functional
endoscopic sinus surgery in the majority of patients, achieving better
quality of life in the long term.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers

Comments
Post a Comment