Spontaneous Regression of a Large Symptomatic Calcified Central Thoracic Disc Herniation: A Case Report with a Review of the Literature-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Abstract
Disc herniations in the thoracic spine are rare and
the incidence of symptomatic thoracic disc herniation (TDH) is 1 in a
million. The incidence of asymptomatic TDH varies from 11-13%. They are
classified as small (≤10%), medium (11-20%), large (21-40%), or giant
(≥41%) based on the extent of canal compromise on advanced imaging. The
large symptomatic calcified central TDHs are best treated operatively,
as the disc fragment could be adherent to the dura or remain intra-dural
[1]. We hereby report a case of one such large central calcified TDH at
the T7-T8 level in a 46 year old gentleman who presented with axial
mid-thoracic back pain and right-sided radicular symptoms along the
intercostal nerve distribution, in addition to tingling and numbness in
his lower extremities. The calcified extruded intra-dural disc fragment
regressed spontaneously over two and half months, while the patient was
waiting for a scheduled elective decompression surgery. The relevant MRI
and CT scan images with a review of the salient literature are
discussed. We believe this to be the first such case of a spontaneous
regression of a large symptomatic central calcified TDH to be reported
in English literature that is documented with CT and MRI scans.
Keywords: Disc herniation; Calcification; Thoracic spine; Spontaneous regression; Radiculopathy; MyelopathyIntroduction
The thoracic spine is the least common region to
present with a disc herniation in comparison to cervical and lumbar
regions. Majority of thoracic disc herniations (THDs) are asymptomatic
and detected incidentally on magnetic resonance imaging (MRI). The
incidence of asymptomatic TDH varies from 11-13% [2]. They are
classified as small (≤10%), medium (11-20%), large (21-40%), or giant
(≥41%) based on the extent of canal compromise on advanced imaging
studies (i.e. CT and MRI) [1,3]. Thoracic disc herniations (TDHs) are
rare and most commonly affect the thoraco-lumbar junction, with the
T11-T12 disc being the most frequently herniated due to the greater
spinal mobility and weakness of the posterior longitudinal ligament [4].
Up to 75% of thoracic disc herniations occur below the T8 vertebra, and
herniation of the upper thoracic spine is very rare. A large proportion
of TDHs are asymptomatic and little is known regarding the natural
history of symptomatic TDHs. They affect older individuals most
commonly, and a history of a precipitating event or trauma is often
absent in at least half to two-thirds of the affected individuals [5].
The symptoms are secondary to chronic spinal cord compression with the
calcification of an extruded fragment suggestive of co-existent
degenerative changes. Younger individuals may present with a soft disc
herniation and a history of acute trauma or a precipitating event that
is responsive to non-operative management. Patients with a TDH may
present with axial back pain, radiculopathy, and/or myelopathy with a
neuro deficit. Males are more commonly affected than females, and
surgery is the treatment of choice for large symptomatic calcified
central TDHs [6]. The discectomy of TDHs constitutes 0.15-4% of all disc
surgical procedures and the intra-operative localization of the correct
surgical level is challenging [7]. A spontaneous regression of a large
symptomatic calcified central TDH is rare and no case report exists to
this day to the best of our knowledge in English literature. We hereby
report one such case of a spontaneous resorption of a large symptomatic
calcified central T7-T8 TDH in a 46 year old gentleman with relevant MRI
and CT image illustrations. A review of the relevant literature with
some of the proposed theories explaining such a spontaneous regressive
phenomenon is also discussed.
Case Report
A 46 year old, right hand dominant academician
presented with a seven month history of axial mid-thoracic back pain
with discomfort and occasional radicular pain around the right
hemi-thorax to the senior author’s office (MRP). The pain was associated
muscle spasms on the right side of midline
that warranted the intake of non-steroidal anti-inflammatory
drugs (i.e. NSAIDs). He had tried a structured physical therapy
program and chiropractic treatment for few months, which
was marginally helpful in alleviating his symptoms. The pain
was aggravated during activities that involved vibration and
jarring (especially travelling), and his symptoms were partially
relieved with rest and NSAIDs. Increasingly, over the recent three
months, he began getting tingling and numbness in his lower
extremities that initiated this consultation in our office. His
Oswestry disability index (ODI) at the first clinic visit was 32%.
The back pain: radicular hemi-thoracic pain ratio was 70:30
at the time of his first consultation. He denied co-existent red
flag signs (i.e. bladder or bowel involvement and foot drop). His
past medical history was significant for arthritis, hypertension,
and type II diabetes mellitus. His past surgical history included
a herniorraphy in his early twenties for an inguinal hernia. He
was otherwise in good health and denied any recent history
of weight loss, night pains, loss of appetite, fever with night
sweats, or chills and rigors. At his most recent annual physical
check-up, the assessment by his primary care physician was
negative for any concerns of malignancy, hemochromatosis,
hyperparathyroidism, gout, pseudogout, and hypercalcemic
states. His personal history was negative for the use of tobacco
products and his alcohol consumption was minimal (<3 drinks
per week).
On clinical examination by the senior author (MRP), he had
some midline tenderness in the mid-thoracic region over the
spinous processes with a good range of motion (ROM) of both
the cervical and lumbar spine. Motor strength testing revealed
normal strength, tone and power (i.e., Medical Research Council
[MRC] grade 5/5 motor strength) in his lower extremities. He had
right-sided radiculopathy/anterior-chest band like discomfort
with hemi-thoracic tenderness along the course of the T7-
T9 dermatomal distribution. His right shoulder and scapular
function were normal and negative for intrinsic shoulder
pathology. The deep tendon reflexes in his knees and ankles were
normal. The Romberg’s sign was negative, his gait was normal,
and he effortlessly performed tandem-walking.
A working diagnosis of a potential space occupying lesion
(SOL) in the thoracic region, causing mechanical compression
of the spinal cord and/or nerve root(s), was suspected. An
immediate MRI scan was arranged, which revealed a large mass
causing the ventral effacement of CSF flow / signal at the T7-
T8 level. His T2 weighted MRI images are illustrated in (Figure
1a & 1b). The differential diagnosis included disc herniation
and other benign intra-axial neoplasms (i.e. meningioma and
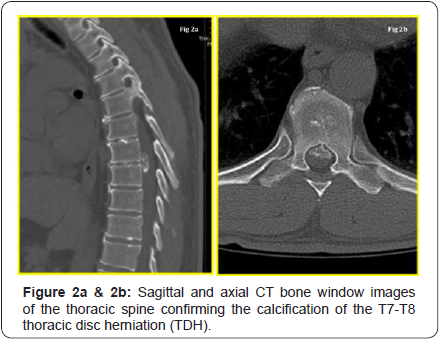
schwannoma). A CT scan was requested to further understand
the lesion, study the extent of calcification / bony, and the intradural
involvement (if any). The key CT sagittal and axial images
are depicted in (Figure 2a & 2b). From these, the diagnosis
narrowed down to a large central calcified TDH, following a
discussion at the multi-disciplinary team (MDT) meeting.

The patient was seen at the office a week later to discuss
the results of his CT and MRI scans. The natural history of disc
herniation, available treatment options, risks, complications,
prognosis, including watchful waiting, were extensively discussed.
Surgical management, using an anterior trans-thoracic approach
with a vascular co-surgeon for access, was discussed at length.
A surgical discectomy with decompression was recommended
and offered, given that he was persistently symptomatic with
lower extremity tingling and numbness for at least three
months, and because non-operative treatment failed. He chose
to electively schedule the surgery in two months (seeking time
off work for his post-operative recovery and making alternative
arrangements for his academic/professional commitments)
with an understanding that it would be undertaken immediately
should there be a change in neurology and/or any bladder and
bowel involvement.
He was seen in the pre-assessment clinic two weeks prior to
the scheduled surgical date, reporting spontaneous improvement
in his back pain and anterior-chest band like tightness, and with
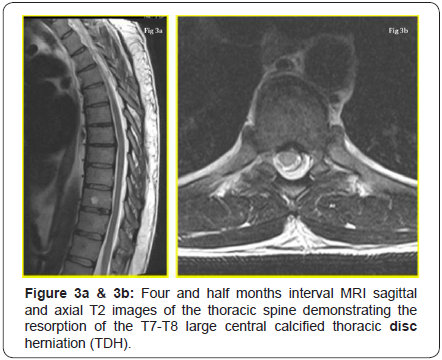
a resolution of his lower extremity tingling/numbness. His ODI was 4%. The proposed surgery was withheld and an interval MRI
scan of his thoracic spine was requested. The T2 weighted images
at two months from his initial MRI revealed the regression of
the large central calcified TDH and this is illustrated in (Figure
3a & 3b). He had a complete resolution of his symptoms while
waiting for surgery and he had normal neurology.He signed a
written consent form and permitted us to submit and publish his
clinical course of events as a case report provided he remained
anonymous.
Discussion
We have reported a case of a large central calcified TDH that
has spontaneously regressed over four and half months while
the patient was waiting for surgical decompressive surgery. The
treatment of choice for a symptomatic large central calcified TDH
is operative excision by the anterior trans-throacic approach [8].
Spontaneous regressions of such central calcified discs are very
rare and we believe this to be the first such reported case in
English literature. The only other case report we could identify
in English was a calcified right-sided foraminal T7-T8 TDH with
a nucleus pulposus calcification in a 36 year old woman that
regressed spontaneously over three months, as reported by
Piccirilli et al. [9]. Though interestingly, our case also had the
disc herniation occur at the same level (i.e. T7-T8), but it was
strikingly different and unique in several aspects, in that our case
had
- A large central calcified TDH,
- The absence of nucleous pulposus calcification, and
- A decade older male patient (46 year old gentleman vs. 36 year old woman).
The pathogenesis of this rare phenomenon of spontaneous
resorption is poorly understood. Proposed theories postulated
to explain it include [10-12]:
- Dehydration of the herniated fragment and its subsequent resorption,
- Activation of the inflammatory process leading to degradation and resorption,
- Re-accommodation of the nucleus pulposus in the inter vertebral disc space, or
- The bathing of extruded disc material in epidural space by blood vessels, which facilitate neovascularisation and eventual macrophage infiltration with phagocytosis.
The clinical course of a TDH is variable, and a patient can
present with non-spinal symptoms and an atypical pain pattern
mimicking other organ system involvement to frank myelopathy.
Though the spinal cord is smallest in diameter in the thoracic
region, the cord: canal ratio is at least 40% compared to 25%
in the cervical region, which make sit sensitive to compressive
effects [4]. Varying degrees of myelo-radiculopathy, Brownsequard
syndrome to paraplegia are reported with symptomatic
TDHs [13]. The incidence of bladder and/or bowel involvement
in TDHs varies from 15-20%. A high degree of clinical suspicion,
supplemented by a thorough history, physical examination, and
confirmation by the appropriate diagnostic imaging, is essential
for accurate diagnosis.
Calcification of inter vertebral discs could potentially occur
at three places:
- The annulus fibrosus,
- The fibro cartilaginous plate, and
- Centrally in the nucleus pulposus.
Von Lushka was the first to describe this phenomenon
in adults and observed such calcifications, especially in the
annulus fibrosus, to be almost always asymptomatic [14].
The calcification of the nucleus pulposus is secondary to the
deposition of amorphous calcium salts in degenerated tissue
and might regress spontaneously, especially in children. Disc
calcification also correlated significantly with the morphologic
degree of degeneration. CT myelography is considered to be the
investigation of choice for the evaluation of calcified TDHs, as it
demonstrates the degree of canal encroachment / intra-dural
extension better than other imaging modalities [15].
Giant TDHs occupy at least 40% of the canal dimensions
and were first defined by Hott et al. [3]. They produced severe
neurological deficit and were associated with poor functional
outcome compared to small and medium TDHs. The authors
recommended open thoracotomy, rather than thoracoscopy, in
treating such giant calcified TDHs. Barbanera et al. [16] reported
a series of 7 patients who had symptomatic giant calcified TDHs
and none of them regressed spontaneously. Brown et al. [17]
evaluated 55 patients with symptomatic TDHs and observed only
15 patients needed surgery (27%). Encouraged by those findings,
they recommended a less aggressive surgical approach, as TDHs did not necessarily cause severe neurological compromise. Wood
et al. [2] studied the natural history of asymptomatic TDHs
and recommended mere observation to be justifiable, even in
symptomatic individuals whose chief complaint was axial spinal
pain. Outside of English literature, we identified only four cases
(three publications) of a spontaneous resorption of a TDH in the
French and Italian languages.
Coevoet et al. [18] reported a case of a T9-T10 protrusion that
regressed spontaneously over 13 months. Martinez-Quinone et
al. [19] reported a case of a T6-T7 TDH in a 47 year old male that
regressed spontaneously. Neither of the two reports specified if
those discs were calcified. Eap et al. [20] reported two cases of a
spontaneous resorption of a calcified TDH. They included a left
T8-T9 foraminal herniation in a 48 year old and a large central
T12-L1 herniation (similar to our case) in a 45 year oldpatient.
Komori et al. [21] observed extensive rim enhancement on
follow-up MRI imaging to be predictive of spontaneous resorption.
A gadolinium enhanced diethylenetriaminepentaacetic acid (Gd-
DTPA) MRI could be used to evaluate the neovascularisation zone
and might give an insight into the dynamics of disc resorption.
Auito et al. [22] studied the determinants of spontaneous
resorption in lumbar disc herniation by longitudinal Gd-DTPA
enhanced MRI scans, focusing on the rim enhancement zone, and
they observed that a higher rim enhancement thickness, a higher
degree of HNP displacement, and the age group of 41-50 years to
be associated with better resorption rate. The clinical symptom
alleviation correlated well with the rate of disc resorption,
and dramatic clinical improvement was seen at the end of two
months. Unfortunately no such studies have been reported until
now for TDHs.
Conclusion
In summary, a large symptomatic calcified central TDH can
be treated with careful observation, as long as the patients
are capable of coping with the pain and do not have any lower
extremity motor weakness or other red flag signs. A better
understanding of pathomechanisms that attempt to further
elucidate the complex interplay between disc calcification,
disc angiogenesis, and disc degeneration is desired, so that
strategies are developed to predict disc herniations that regress
spontaneously. Studies focusing on investigating such link
mechanisms are desired and constitute grounds for further
research. Such studies might also explain which TDHs would
most likely regress on their own and define the role of surgery
vs. non-operative treatment in the management of symptomatic
large central calcified TDHs.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
Comments
Post a Comment