Platysmal Myocutaneous Flap for Reconstruction of T1,T2 Tongue Cancer: Functional Assessment-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF HEAD NECK & SPINE SURGERY
Introduction
The platysma myocutaneous flap (PMF) was first used
for intraoral reconstruction in 1978 by Futrell (Futrell et al., 1978)
[1]. A platysma myocutaneous flap is a versatile, easy-to-perform,
one-stage procedure, and the outcome is best in adequately selected
patients, with minimum donor site morbidity. It is large enough to close
most head and neck ablative skin or mucosal defects up to 70cm2 and no
special equipment is required (Koch, 2002) [2]. The PMF is also an
excellent alternative choice to microvascular flaps, especially in
patients who are medically unfit for prolonged surgery [3]. But PMF is
not as popular as other options of head and neck reconstructive, because
of different reasons. The main limitations are lack of bulk,
problematic blood supply and unreliability. Also the rates of
complications between 10% and 40% have been reported, which includes
partial or complete necrosis, fistula, dehiscence, hematoma and
infection [4]. The rates of complications have been linked to surgeon’s
experience, technique followed and other preoperative factors. In this
study we describe our experience with the use of PMF in reconstruction
of T1, T2 malignant lesions of tongue. The main objective of our study
is to evaluate the feasibility of PMF in tongue reconstruction. And also
to evaluate the functional outcome in terms of speech and swallowing,
after tongue reconstruction with PMF.
Materials and Methods
In this descriptive study, a total of 75
non-consecutive patients of T1 and T2 tongue cancer, undergoing
treatment at Dharamshila Narayana superspeciality Hospital, New Delhi
were retrospectively evaluated by collecting data from the period from
2013 to 2016. In our series, newly diagnosed squamous cell carcinoma
cases of tongue malignancy of only T1 and T2 lesions
with no previous surgery and radiotherapy were included. All patients
underwent adequate glossectomy and modified radical neck dissection.
Histologically, we confirmed tumor free margin of resection by using a
frozen section technique. The size of the flap was designed according to
the anticipated defect resulting from the excision of the primary
tumor.
Operative procedure
In this descriptive study, a total of 75
non-consecutive patients of T1 and T2 tongue cancer, undergoing
treatment at Dharamshila Narayana superspeciality Hospital, New Delhi
were retrospectively evaluated by collecting data from the period from
2013 to 2016. In our series, newly diagnosed squamous cell carcinoma
cases of tongue malignancy of only T1 and T2 lesions with no previous
surgery and radiotherapy were included. All patients underwent adequate
glossectomy and modified radical neck dissection. Histologically, we
confirmed tumor free margin of resection by using a frozen section
technique. The size of the flap was designed according to the
anticipated defect resulting from the excision of the primary tumor.

The anticipated skin paddle was outlined in the
lower anterio-lateral neck making it an island. The parallel vertical
incision was outlined, starting at the chin medially and the tip of the
mastoid process laterally with extension of 2 to 2.5cm above the
clavicle bone inferiorly. Depend the skin incision of designed skin
paddle up to platysma muscle. Complete the neck incision from chin to
mastoid tip and up to platysma muscle.Separate the myocutaneous paddle
in supra platysmal plane by
sharp dissection up to angle of mandible. External jugular vein
is isolated for purpose to take it along the flap in subplatysmal
plane for adequate venous drainage. Then elevate the paddle of
flap in subplatysmal plane in an inferior to superior direction
taking care to avoid underlying fat and lymphatic tissue with flap.
Meticulous and sharp dissection preferably with bipolar cautery
is done while removing submandibular gland and preserve facial
vein and facial artery intact with its submental branch which
serve as main arterial supply to flap [5] (Figure 1).
Post operatively, patients are evaluated for a period of six
months to one year and assessment of tongue mobility, speech,
swallowing, and surgical complications of flap as well as neck
wound were done.
Speech was evaluated by AYJNIHH 7- point speech
intelligibility rating scale [6].
This 7- point rating scale is as follows:
- No noticeable differences from normal.
- Intelligible though some differences occasionally noticeable.
- Intelligible although noticeably different.
- Intelligible with careful listening although some words unintelligible.
- Speech is difficult to understand with many words unintelligible.
- Usually is unintelligible.
- Unintelligible.
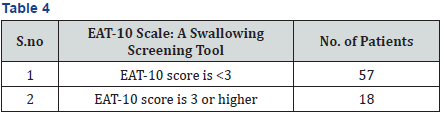
Swallowing assessment was done by EAT-10 scale [7]. This
scale rates swallowing function, based on the patient’s responses
to questioning, on scale maximum points of 40. If the EAT-10
score is 3 or higher, it indicates swallowing difficulties. This scale
have 10 questions with a score of 0 to 4. The score 0 indicates
no problem and score 4 indicates severe problem. As the score
increases the severity increases.
The questionnaire is as follows:
- My swallowing problem has caused me to lose weight (0-4).
- My swallowing problem interferes with my ability to go out for meals (0-4).
- Swallowing liquids takes extra effort (0-4).
- Swallowing solids takes extra effort (0-4).
- Swallowing pills takes extra effort (0-4).
- Swallowing is painful (0-4).
- The pleasure of eating is affected by my swallowing (0-4 )
- When I swallow food sticks in my throat (0-4).
- I cough when I eat (0-4).
- Swallowing is stressful (0-4).
Tongue mobility is evaluated by asking patient to touch the
upper lip, right commisure and left commisure with tip of the
tongue. The surgical complications of flap that are assessed,
include partial and complete loss of flap, flap detachment,
marginal necrosis, fistulisation and partial epidermolysis.
The neck wound healing status is also evaluated as follow:
normally healed, wound dehiscence, skin flap necrosis and
wound contraction. The criterion used to differentiate between
extended or regular wound dehiscence was the presence of a
“dehiscent area” ≥ 2cm2. Skin flap necrosis was defined as wide
when it affected an area of 2 cm2 or more [7].
Mobility of tongue (To upper lip/Right commissure/Left
commissure): Tongue mobility evaluated by asking patient to
touch the upper lip, right commisure and left commisure with
tip of the tongue.
Results
A total of seventy five patients with T1 and T2 tongue
cancer were included in the study. The histologic diagnosis was
squamous cell carcinoma in all cases. All patients underwent
curative Adequate glossectomy with modified radical neck
dissections. Complications of the flap, Status of the neck Flap,
Swallowing and speech function and tongue mobility were
evaluated 6 months to 1 year postoperatively.
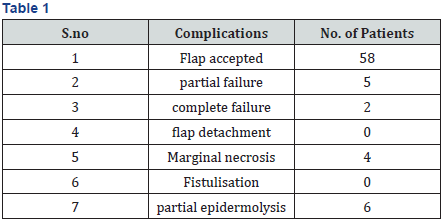
Complications of the flap
Flap complications were noted in 17 patients (22.6%) with
complete failure in 2 patients (2.6%), which was managed
by complete wound debridment and allowed healing with
secondary intension. Partial failure in 5 patients (6.6%) was
managed by local measures, such as surgical wound debridement
of necrotic tissue. Marginal necrosis and partial epidermolysis is
seen in 4 patients (5.3%) and 6 patients (8%) respectively. These
complications need prolonged nasogastric nutrition for 15 days
(Table 1).
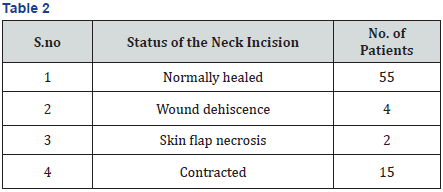
Neck wound complications
Neck wound complications were divided into four categories
in which 55(73.3%) cases had normal healing of neck incision flap (Figure 2). Wound dehiscence and skin necrosis reported
in 4(5.3%) and 2(2.6%) respectively, required surgical revision.
Most of the patients 15(20%) reported with contraction and
neck stiffness which was treated by neck physiotherapy (Table 2).
Speech
After excision of primary lesion and platysma flap
reconstruction, intelligibility fell to grade 6 in two (2.6%) patient,
Grade 5 in three (4%) patient, and grade 4 in five (6.6) patients.
More patients showed intelligible although noticeably different
in 27(36%) patients and intelligible though some differences
occasionally noticeable in 38(50.6%) patients (Table 3).
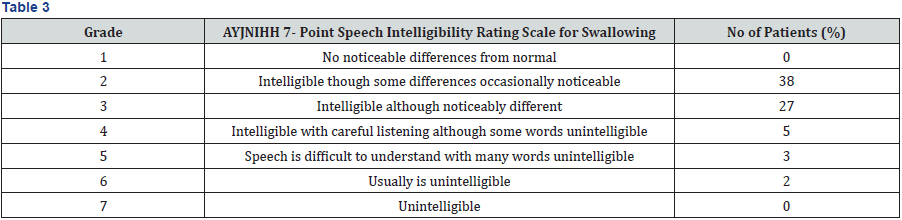
(“1” = no noticeable differences from normal, “7” = unintelligible).
Swallowing

Mobility of tongue
In these adequate glossectomy patients with platysma
flap reconstruction, tongue mobility was evidently recovering,
and mostly adequate for producing intelligible speech. Tongue
mobility in Upper lip, Right commissure, and Left commissure
seen in 47 (62.6%) patients. One side restricted movements
mostly towards reconstructed site in 13(17.3%) patients.
Two side restricted movements and completely restricted
tongue mobility is seen in 9(12%) patients and 6(8%) patients
respectively (Table 5).
Discussion
The primary blood supply to PMF derives from sub mental
artery which branches from a facial artery and additional blood
supply comes inferiorly from the cervical transverse vessels,
medially from thyroid vessels and laterally from occipital and
postauricular vessels. This is a multiaxial blood supply as it has
multiple anastomoses with ipsilateral and contralateral mental,
labial and sublingual arteries [8-10].
In our study of the 75 patients we preserve the facial
artery and external jugular vein. External jugular vein provides
retrograde valve less communication with internal jugular vein
through retromandibular and facial venous system, which allows
adequate venous drainage.
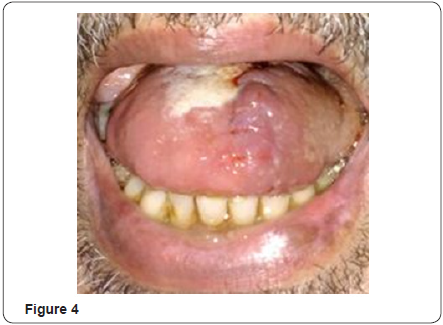
The experience about reliability of platysma flap is not
uniform among the various authors, some author claim excellent
results, while others experienced the poor results [11]. Our
results showed 77.3% of complete acceptance of the flap (Figure
3-5) while remaining 2.6% shows complete failure(2cases) and
6.6% (5 cases) were partial loss of the flap. Marginal necrosis and partial epidermolysis is seen in 4 patients (5.3%) and 6
patients (8%) respectively. The rates of necrosis of platysma
myocutaneous flap found in many other studies ranged from 7.1
to 29.2% [11].


In tongue reconstruction, restoration of speech is an
important component. After excision of primary lesion and
platysma flap reconstruction, intelligibility fell to Grade 6 in only
two (2.6%) of patients, Grade 5 in three (4%) patients, and grade
4 in five (6.6) patients. Majority of patients showed Grade 3
(intelligible although noticeably different) patients and Grade 2
(Intelligible though some differences occasionally noticeable) in
patients. Similar results were reported in a study where majority
had speech restoration without significant deficits in a month
after surgery [12].
Thin and pliability of this flap allows reconstructed tongue
with good mobility. Good mobility of tongue is seen in 47(62.6%)
patients and restricted tongue mobility is seen in 15(20%).
Conclusion
In conclusion, surgeons should consider the option of using
a platysma myocutaneous flap when reconstructing tongue
defects. The main advantages are that this flap is readily available,
easy to perform, can be obtained during neck dissection and the
donor site can be closed in a primary way, with minimal flap
complications and good functional outcome. Results can be
compared with free flap reconstruction.
To know more about Open Access Journal of
Head Neck & Spine Surgery please click on:
To know more about Open access Journals
Publishers please click on : Juniper Publishers
Comments
Post a Comment