Simulation in ENT- Is There a Place For It?-Juniper publishers
Introduction
Airway emergencies are a common presentation in the
emergency department, with the incidence reported to range between 2%
and 14.8% Kovacs et al. [1]. In the vast majority of cases, ‘difficult
airway’ presentations are managed successfully by emergency medicine
doctors Wong et al. [2]. While anaesthetic staff on the whole manage the
remainder, surgical doctors (especially those working within ENT
surgery) are often involved in cases that require invasive interventions
such as tracheostomy or surgical cricothyroidotomy Awad et al. [3].
Furthermore, it is often the most junior member of the ENT team is first
to attend to those patients requiring emergency on-call airway
services; frequently without immediate senior supervision or support.
Despite this, there is currently no formal curriculum
in airway management for core surgical trainees (ISCP, 2013) and as
such, training is highly variable. Awad et al. [3] conducted a survey
assessing competence of emergency airway management amongst one hundred
ENT surgical house officers in the United Kingdom and reported that only
54% of respondents felt their training in this area was adequate and
felt confident to provide emergency airway services. Furthermore, the
authors found that attendance at ALS or ATLS courses correlated poorly
with trainee confidence and perceived adequacy of training.
While there is a large availability of airway
management courses, the majority appear to be aimed at the anaesthetic
audience. Of those available to alternative groups, most are either too
basic or too advanced to meet the requirements of the core surgical
trainee working in ENT [4].
Rationale for simulation
Training in medicine has traditionally been based
upon an apprenticeship model whereby the novice is taught by an ‘expert’
(usually within the clinical arena); ultimately becoming master
craftsman him or herself Chur H et al. [5]. However, such a model has
been significantly challenged by a number of factors including the
European Working Time Directive and its impact on available training
time, variability in trainee exposure and increased emphasis on patient
safety Motola et al. [6]. Such concerns may in part be responsible for
the exponential rise of simulation training within medical education
over the past two decades.
Simulation-based medical education (SBME) enables
trainees to learn within a safe, controlled environment without
compromising patient safety [7-9]. In addition, SBME offers the
opportunity for formative assessment and feedback. The basis of
simulation is underpinned by the concepts of deliberate practice and
mastery learning; the former refers to the identification and practice
of specific components of a skill, which provides immediate feedback to
promote improvement Ericcson [10]. Ericcson (2004) argues that
deliberate practice is critical to the acquisition of motor skills and
pivotal to the transition from competency to expertise. Indeed,
Ericcson’s research highlights that deliberate practice is a more
powerful predictor of expert performance than is academic aptitude or
experience. Deliberate practice is of particular importance when
considering motor skills that are rarely performed (i.e. emergency
surgical cricothyroidotomy) and thus offers little opportunity for
practice within the clinical setting. The concept of mastery dates back
to 1960s Motola et al. [6] and has its origins in engineering education.
In essence, mastery learning is competence-based
education that aims to ensure all learning objectives are attained by
all learners; eliminating variation in trainee outcomes as far as
possible Wong & Kang [11]. However, it is acknowledged that learners
may take varying amounts of time to achieve mastery [12]. A number of
authors have documented various positive translational outcomes of SBME
including reduced length of hospital stay, fewer intensive care
admissions as well as reduced health care costs Barsuk et al. [13]. For
instance, a recent systematic review undertaken by Cook et al. [14]
comparing mastery SBME with traditional training within healthcare
reported that SBME had a large and statistically significant effect upon
skill acquisition and a moderate effect upon patient outcomes.
Curriculum
A hybrid SBME program that incorporates an initial
didactic lecture, skill stations and intermediate-fidelity simulation
scenarios with the focus on the recognition and management of airway
compromise, aimed specifically at junior surgical
trainees working within ENT surgical departments is proposed.
As a prerequisite, participants should be working within an ENT
department and have completed both ALS and ATLS. Although,
a number of airway management courses are already currently
available, these appear not to include all the elements outlined
above. Furthermore, the vast majority may be arguably too basic
for the junior surgical trainee working within ENT surgery (i.e.
ALS), or indeed too advanced; being aimed at anaesthetic or
ENT specialty trainees. The course will not only aim to teach
participants the technical skills required to manage patients
with airway compromise, it will also address the non-technical
elements through the use of simulation scenarios.
This will be performed in a three-step manner whereby
participants can build open their knowledge by first providing the
opportunity to learn or review underlying theoretical principles
of airway management, followed by the practice of specific skills
or procedures, before finally applying such knowledge and skill
later within the simulation scenarios. Windsor [15] outlines
a hierarchy of surgical skill acquisition beginning with basic
or core skills, becoming more complex and automatic with the
attainment of procedural and non-technical skills. Professor
Windsor, a surgeon himself, emphasises that in traditional
surgical training, the trainee is expected to master skills from
all such domains simultaneously. He follows further that SBME
enables trainees to learn appropriate skills at a time that is
appropriate to their experience. This is somewhat in keeping
with Bloom’s Taxomony of Learning 1956 cited in Amer [16] that
outlines three educational domains as cognitive (knowledge),
psychomotor (skills) and affective (attitudes) and follows that
educators and the learning activities they use should facilitate all
levels of learning commencing with the most basic and building
to a level which ultimately fosters high cognitive education [17].
Skills stations
The trainees will rotate through three skills stations in small
groups. Each station will be led by one senior clinician and will be
interactive to enable participants to discuss and clarify ideas and
issues. Each station will provide the opportunity for ‘hands on’
practice in basic airway skills (simple adjuncts) and intubation,
surgical airways (cricothyroidotomy and tracheostomy) and
fibro-optic nasoendoscopy. Skills will be performed on cadaveric
head and neck specimens [18-20].
Intermediate-fidelity simulation
Skill stations will be followed by a series of simulation
scenarios using a Sim Man patient simulator; all with the theme
of management of patients with rapidly deteriorating airway
problems. The scenarios will be formulated from a combination
of real life examples and learning needs assessments.
Participants will undertake simulation scenarios individually,
playing their true role as ENT surgical house officers and will be
assisted by other participants and facilitators who will assume the role of nursing and anesthetic staff to increase the realism
of the scenario. Realism is important in fostering the notion of
suspension of belief whereby participants ‘buy into’ the scenario
as a real life clinical situation [21-23]. Each scenario will last 8-10
minutes in duration and will be preceded by a concise briefing in
the form of a referral or handover. The remaining participants
will follow the progress of each scenario via a live video feed.
The simulation scenarios will not only provide an opportunity
for participants to transfer and apply the knowledge and skills
acquired from the previous activities it will also assess candidate
ability to function as an effective team member. In modern
medical practice, there is increasing emphasis being placed upon
the impact of the clinical environment, wider team dynamics
and human factors Marshall & Flanagan [24] and it has been
shown that effective team working is an essential component
of care delivery and overall patient outcomes. In particular,
communication, or more specifically, miscommunication was
indicated as a root cause of almost 70% of significant events Joint
Commission of Sentinel Events [25]. Despite this, undergraduate
and early surgical education has traditionally failed to address
the skills required to work effectively within teams; focusing
primarily on knowledge and acquisition of technical skills
Flanagan et al. [26].
Debriefing and feedback
Feedback is an integral aspect of learning within SBME. Van
De Ridder et al. [27] define feedback as an activity that involves
the giving of specific information around a trainee’s observed
performance given with the intent to improve their performance.
Debriefing is a specific form of feedback employed in SBME
and has been described as the single most important part of
simulation training Rall et al. [28]. The importance of debriefing
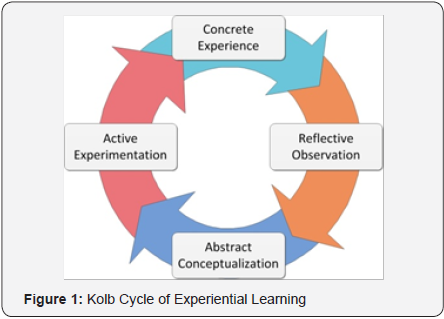
and feedback can perhaps be explained again by the work of
Kolb’s four-stage model of experiential learning (1984 cited in
Motola et al. [6]) that reinforces that enhanced learning occurs
when participants are given feedback to form the basis of a postreflective
process where they are able to make sense of events
through analysis and subsequently implement new ideas and
theories to facilitate improvement (Figure 1).
Savoldelli et al. [29] support this highlighting that isolated
simulation encounters without feedback often fails to lead to
trainee improvement, particularly in the domain of non-technical
skills. It must however be borne in mind that feedback has the
potential to be demoralising and counterproductive; having a
negative impact upon learning if delivered ineffectively Wulf et
al. [30]. Given the importance of debriefing, a significant amount
of time will be allocated to undertaking this process (up to 40
minutes for each scenario) and will be undertake as a group
activity facilitated by two instructors [31].
Conclusion
Although it is clear that simulation in health care can
be effective, to date empirical evidence around aspects of
development, instructional design as well as implementation of
simulation programs is largely lacking. With specific reference to
SBME in surgery, there is strong evidence that simulation is an
effective educational activity for the acquisition of surgical and
non-technical skills. More specifically, SBME is also proving to
be important in airway management education and as such may
be an invaluable adjunct to the current ENT specialty training
curriculum. Within core surgical training where no formal
curriculum exists around acute airway management however,
simulation may offer the only opportunity for formal teaching
before junior doctors working in ENT are faced with a real life
patient with airway compromise.
To know more about Journal of Head Neck please
click on :

Comments
Post a Comment