Latex Allergy: Overview and Recommendations for the Perioperative Management of High-Risk Patients-Juniper Publishers
Juniper publishers-Journal of Head Neck
Latex is a natural substance that comes from the sap
of the rubber tree. It is a material widely used in the manufacture of
domestic, industrial and especially medical products [1]. The prevalence
of latex allergy in the general population is estimated between 0.8 and
6.5% [2], and the repeated exposure to this material is the most
significant risk factor for its development [3]. Among the main risk
groups are health personnel, where the incidence reaches 17%, and
patients with spina bifida where 73% incidence has been described [4]
(Table 1). Factors as age, race or sex are not associated with an
increase in risk.

Worldwide, it is estimated that in one of every 3.500
to 20.000 surgeries an anaphylactic reaction occurs, which
represents about 9% to 19% of all surgical complications, with a
mortality varying between 3% and 9% [5]. About 50% of the medical
devices contain latex [6], so it is not a surprise that this material is
the second cause of perioperative anaphylaxis, being responsible in the
12 to 16.7% of cases [7]. Fortunately, this incidence has decreased
significantly since hospitals and outpatient surgery facilities have
adopted latex-free policies [5]. Based on this background, latex allergy
is a condition of special interest to the healthcare professionals.
This review of the literature seeks to expose the relevant basic
concepts about allergic reactions to latex, as well as to generate
guidelines for the perioperative management of sensitized patients.
Sensitization mechanisms and immunological associated to latex reactions
Latex allergy is associated to any
immunologically mediated reaction to this material, associated with
clinical symptoms. Since the 1980s, there has been an increase in the
incidence of allergic reactions to latex, associated with the
introduction of mandatory use of gloves within universal precautions in
the prevention of infectious diseases such as HIV, Hepatitis B and C
[1,3,8]. Sensitization depends on factors such as the route, dose,
frequency of exposure, and individual susceptibility [2,4,9]. Exposure
may occur as a result of direct contact with skin or mucous membranes, a
wound inoculation, or ingestion.
Another type of exposure occurs when the latex proteins
bind to the dust that contain these products, volatilizing during
the placement and removal of gloves, being inhaled and to enter
the respiratory tract [10].
It has been shown that these particles can remain suspended
in the environment for up to 5hours [4,11]. The amount of
exposure needed to sensitize a person is unclear, and the
threshold required to trigger an allergical response varies
considerably among individuals [12,13]. Is possible to describe
three types of allergic reactions to latex:
Irritant contact dermatitis: It is the most common type
of allergic reaction. Can develop within minutes or hours after
exposure, due to mechanical or chemical skin irritation by the
components used in the product manufacturing process [3].
Clinically it is characterized to present as pruritus, rash, scaling,
burning sensation, inflammation or blistering [8]. No previous
sensitization is necessary for the development of dermatitis,
but this condition facilitates the progress of an immunologically
mediated hypersensitivity reaction, because the lost of skin
integrity favors the direct exposure to allergens [14].
Allergic contact dermatitis or type IV hypersensitivity
reaction: Reaction mediated by cellular immunity. It occurs
between 6 and 48hours after contact with latex, but is usually
produced by other allergens from the chemicals used in the
production process [8]. T lymphocytes are sensitized and
infiltrate the contact zone on the skin [1]. The symptoms are
similar to those of irritative contact dermatitis (erythema,
vesicles and desquamation) and do not require a history of
previous contact to manifest itself [7].
Type I hypersensitivity reaction: It occurs after minutes
of exposure, either by the cutaneous, mucosal or aerial route. It
requires prior sensitization with latex proteins and production
of IgE antibodies. Clinically, it can present as a localized urticaria
to a frank anaphylactic reaction. Moderate reactions include
rhinitis and conjunctivitis, and are more likely to occur due air
exposure or skin contact.
Eighty percent of the reactions associated to latex correspond
to contact dermatitis or type IV hypersensitive and occur mainly
in response to chemicals used in the manufacture of these
products [12]. Only type I hypersensitivity corresponds to a
response to proteins in the latex [8]. This reaction is less frequent
but can generate large complications and life threatening if it is
developed during the perioperative period.
Identification of allergic patients or at potential risk
High-risk populations are those that are frequently exposed
to latex elements, such as patients undergoing multiple surgical
procedures, health personnel, rubber workers, and individuals
with a history of atopy [1]. These populations are at increased
risk of developing more frequent and severe allergic reactions
[5]. In particular, patients with congenital malformations of
the central nervous system give especial interest. In patients with spina bifida, incidence of latex allergy has been reported
in 35% to 73% [4,15]. These patients have also show increased
sensitization to latex protein and a significant increase in levels of
fully and specific latex IgE from the perinatal period, which could
be associated with the occurrence of allergy in the future [16].
Another example is patients diagnosed with myelomeningocele,
with an estimated incidence of 19.51% latex allergy, and 18% of
sensitized patients [17]. The most important risk factor to the
development of allergy in these cases is the history of 5 or more
surgical interventions [17,18].

Deep clinical history minimizes the risk of new exposure
in sensitized individuals during prior medical and dental
procedures. The anamnesis should emphasize on risk factors,
such as exposure to latex, spina bifida, reconstructive urologic
surgery, multiple surgical procedures, intolerance to latex
products [balloons, gloves, preservatives, dental rubber dams),
allergy to fruits, history of intraoperative anaphylaxis of unknown
cause, or health personnel with a history of atopy [4] (Table
2). It is estimated that in 30% of cases of anaphylaxis, there is
a suggestive history of previous reactions [7]. Individuals with
allergies to some specific foods are at increased risk of develop
allergic reactions to latex. Although the mechanism is not clear,
some proteins present in certain fruits may act similarly to the
latex allergenic proteins and produce sensitization [1]. It has
been reported that between 21.2% and 86% of patients with
documented allergy to latex also had a food allergy. Some of
the foods that could produce cross-reaction with latex include
banana, avocado, kiwi, grapefruit, papayas, almonds, chestnut,
pineapple and tomatoes among others [6]. Allergy to these foods
may precede allergy to latex or vice versa.
Prevention Strategies
The best treatment is to avoid exposure [1,12]. The incidence
of anaphylactic reactions to latex has decreased due to the
identification of high-risk patients, better diagnostic tests and
preventive measures [3]. For patients with spina bifida treated in latex-free environments, incidence of latex allergy seems to
be similar to the general population. More specifically, it has
been reported an incidence of 5% sensitization and 0.8% of
allergies in patients with spina bifida hospitalized in latex-free
environments, versus 55% and 37%, respectively, in patients
managed in environments without restriction to exposure to
latex [19].
Given that in most cases is not feasible to have 100% latex-free
environments, is essential to at least generate a safe environment
for patients with prior allergy history to this material. This is
usually sufficient and is more achievable than an environment
completely free of latex [11]. These general measures include
adequate identification of allergic patients, proper labeling
of products formulated with latex and use of latex-free gloves.
Among the general recommendations for health establishments
is important to educate staff, establish clear protocols for the
management of these patients, have a latex-free cart available
and check the latex contents of the entire surgical team.
The antigen content in latex products can vary significantly.
Products manufactured with an “immersion” process (eg
gloves and preservatives) have the highest levels of allergens,
whereas dry rubber (eg tires, rubber seals, plugs and plugs of
vials and syringes) are less allergenic [8]. It is important to note
that products labeled as hypoallergenic have fewer chemicals
responsible for causing allergic reactions, skin irritation and
dermatitis, but this labeling is not related to the latex content of
these products [11,14]. The two main prevention strategies are:
Use of latex free gloves: There is important evidence
that latex gloves are the main source of allergens in health
care settings [12]. These have been the most popular given
their characteristics, which include strength, elasticity and
superior protection qualities. It has been shown that the level
of aeroallergens in the environment is strongly correlated with
the use of gloves with high content of allergens and dust, total
number of gloves used and hours of activity in the environment.
Studies have shown that changing gloves with high dust content
by gloves with low amounts or dust-free (which are low in
proteins and allergens) results in a significant reduction of
aeroallergens and a dramatic decrease in the incidence of latex
allergy. It has also been reported that after removing latex
gloves at work sites, the levels of aeroallergens are reduced to
undetectable levels after 24hrs [8].
Concern about latex allergy has led to alternatives such as
polyvinyl chloride (PVC) gloves or nitrile gloves. It seems to be
that PVC gloves filter more than latex gloves (63% filtration
in PVC gloves, versus 7% latex gloves), but on the other hand
nitrile gloves have shown a better performance than those of
PVC. Unfortunately routine use has received some resistance
[12] and latex gloves continue to be a cheap alternative, offering
appropriate protection and other essential qualities for safe and
effective performance.
Pre-medication: The role of pre-medication with H1
antagonists and corticosteroids is not well defined. These
medications may help to decrease non-IgE-mediated reactions.
However, they do not prevent IgE-mediated immune reactions
[7,12,20]. Avoiding exposure to the allergen is the only way to
avoid an anaphylactic reaction.
Surgical Management Protocol for Patients with Latex Allergy [2,4,13]
The following measures are aimed at promoting safe care
during the perioperative period in patients at risk for an allergic
reaction to latex, either by medical history or because they have
positive laboratory tests:
Preparation of the surgical theater and preoperative period [2,13]- The procedure or surgery should be scheduled first thing in the morning, when the levels of aeroallergens are lower.
- Install a label on the door of the operating room that identifies the patient as allergic and to the room as latex-free.
- The day before surgery, remove all products containing latex (reserve bags, endotracheal tubes and laryngeal masks that are not latex-free).
- Cleaning staff of the surgical room should not wear latex gloves. The day of the surgery, the surfaces should be cleaned again to remove the suspended powder.
- When appropriate, the mattress should be protected with double bed sheet.
- Cover all monitoring devices, cables/tubes (oximeter, blood pressure, electrocardiogram) to avoid direct contact with the skin.
- Products sterilized in ethylene oxide must be rinsed before use. Residual ethylene oxide reacts and may cause an allergic response in a patient allergic to latex.
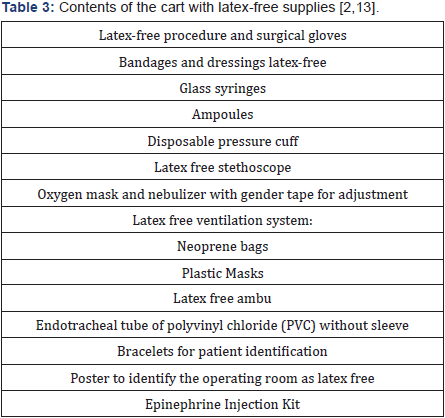
- A cart with latex-free supplies (Table 3) should be available inside the operating room.
- The operating room should be adequately equipped
to handle an unexpected anaphylactic reaction and have
immediate availability of epinephrine.
- Allergic patients should be identified at the time of
admission with: a bracelet, in the medical history and in the
sheets of nursing.
- Before the pressure is taken, the arm should be covered
with a cotton mesh and auscultated through it, avoiding that
the stethoscope has contact with the skin.
- The patient should wear a cap without elastic and
gender boots.
Intraoperative period
- All the surgical team should wear latex free gloves.
- The traffic inside the surgery room should be minimal.
- Do not use penrose drains, latex bands, latex irrigation
elements (eg irrigation pears).
- Latex-free or glass syringes should be used.
- Medications should be preferred in glass ampoules. If
not available, remove the rubber stoppers before preparing
the medication.
- Medications should be prepared immediately prior
their administration to minimize contact with the syringe
plunger.
Postoperative period
- The postoperative period should be performed in the
room prepared for the patient or inside the same operating
room.
- All departments involved must be informed of the
presence of patients allergic to latex, so that they can take
the necessary precautions to protect them.
Detection and management of an allergic latex reaction
Since the allergen is generally absorbed slowly from
the
surgeon’s glove, the reaction usually occurs about 30 minutes
after contact with the skin and mucous membranes during the
maintenance of anesthesia, not during the induction period.
However, the actual start of the reaction may range from 10 to
290minutes [13]. This interval will depend on the sensitivity of
the patient, amount of allergen absorbed and the contact surface
(absorption is faster through the peritoneum or vaginal mucosa
than through the skin) [7]. Except for these characteristics, latex
reactions are similar in their manifestation to those reactions
caused by other agents during surgical and medical procedures
[2] such as muscle relaxants or antimicrobials.
The management of an intraoperative anaphylactic reaction
is well-documented [4,5,13,21] and includes pharmacological
and non-pharmacological measures according to the clinical
presentation, course of the condition and the context in which
anaphylaxis occurs. In the particular case that the reaction
is suspected to be caused by an undiagnosed allergy to latex,
the following measures should be incorporated as part of the
management:
- Stop or minimize the absorption of the agent (consider
the variety of possible routes of exposure).
- Remove all products containing latex and change to
latex-free gloves.
- Place an allergy alert to the latex in a visible place at the
entrance and inside the surgery room.
- Complete the study of the patient after the reaction.
In mild cases, spontaneous recovery may be observed even in
the absence of any specific treatment. In such circumstances, lack
of proper diagnosis and evaluation can lead to fatal re-exposure
[20]. Any suspected hypersensitivity reaction during anesthesia
should be extensively investigated through a detailed history
of the reaction, with emphasis on concomitant pathologies,
known allergies, previous anesthetic history and the stage of
anesthesia were the reaction occurred, in addition to performing
laboratory tests according to each case [7]. Immediate tests have
been designed primarily to determine whether or not an allergic
mechanism is involved in the reaction, while late testing seeks to
identify the drug responsible and possible alternatives to its use
[20]. Among the tests available for the study of latex allergy are:
Serum tryptase: Indication of mast cell activation. It rises
in mediated and non-IgE mediated reactions. A concentration
above 25mcg/ml might suggest a type I reaction [5,7]. The
recommendation is to take serial samples immediately, at 2, 6
and 24 hours, after the reaction. It has a sensitivity of 64% and a
specificity of 89% for anaphylaxis. The absence of a high tryptase
does not exclude an anaphylactic reaction.
Serum-specific IgE: The recommendation to perform
this test after 4 to 6 weeks and before 6 months of the event.
Immediate measurement could give a false negative. The
sensitivity of IgE tests is variable; for latex is about 92%.
Skin tests: They can be done up to one year after the event, but
not immediately to avoid a false negative. The recommendation
is to wait 4 to 6 weeks after the reaction.
Prick test: Evaluates the sensitization to the latex, with a
sensitivity and specificity close to 100% [4]. Only IgE-mediated
reactions can be studied with cutaneous tests [7], since they do
not identify non-immunologically mediated reactions [5].
Patch test: Is recommended for the study of latex contact
dermatitis. Additives used in the glove manufacturing process
should be included, since delayed hypersensitivity is rarely due
to allergens characteristic of unprocessed latex [14].
Conclusion
Although achieving completely latex-free environments is
unrealistic, every effort should be made to minimize the risk
of sensitization, especially in high-risk groups such as patients
with congenital malformations requiring multiple surgical
interventions during their early years of life. In addition, it is
important to consider that achieving an environment with low
levels of allergens is an issue that not only involves the safety
of the allergic patient. The implementation of these measures
has a significant impact on the sensitization of exposed health
personnel and barriers to protection against infectious diseases.
The management of latex allergy should be approached from
different perspectives and multidisciplinary support should be
obtained to:
- Establish policies for the identification and care of patients with known allergy to latex;
- Develop policies and procedures for health workers with latex allergy;
- Provide environmental control and resource management to minimize unnecessary exposure of patients and staff to materials with a high content of latex antigens; and,
- Promote the ongoing training of patients and employees on the topic of latex allergy.
To know more about Journal of Head Neck please
click on :

Comments
Post a Comment